Anterior hepatic resection: a simple and safe new technique for reducing the antero-posterior diameter of the liver graft for small pediatric recipients
Joao Seda Neto1, Carolina Costa1, Nathalia Porto1, Caio Oliveira1, Marcel Benavides1, Renata Pugliese1, Rodrigo Vincenzi1, Karina Roda1, Paulo Chapchap1, Eduardo A Fonseca1.
1Hepatolog and Liver Transplantation, Hospital Sirio-Libanês, São Paulo, Brazil
Background: The use of segmental liver transplantation in children has evolved overtime, from left lateral segments (LLS), hiper-reduced LLS (lateral and/or inferior LLS resections), and use of true monosegments (Segment II), especially in small children and neonatal LT. The aim of this study is to report the initial experience with the anterior LLS resection, in concomitance (or not) with the usual LLS hiper-reduction, in the living donor operation.
Methods: Initially the anatomic bases for the technique were defined through a retrospective anatomic measurement of the available donor pre-operative abdominal CT-scans. Two distances were measured: 1- distance from the emergency of the left portal vein to the liver surface 1cm to the right of the falciform ligament (M1), and 2: distance from the segment III portal vein emergency to the liver surface (M2). Finaly, 3 cases where the anterior liver resection was performed were described. The simple technique consisted in resecting the anterior aspect of the liver 1cm above the position with larger diameter (from the PV to the surface) in direction to the falciform ligament. The procedure was performed after the live donor LLS resection was completed. It was performed in situ, during the donor surgery.
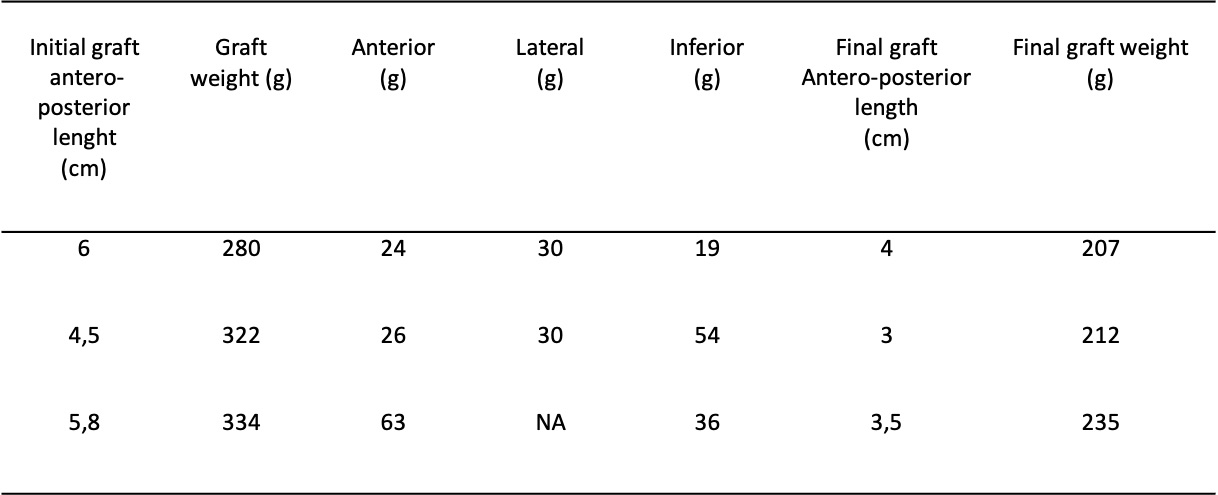
Results: 40/ 144 (27.7%) donors underwent pre-operative abdominal CT-scan. Average M1 and M2 were 5.3cm + 1.0cm, and 2.8cm + 0.5cm, respectively. In the 3 cases where the anterior liver resection was performed, all donors were male, with average BW and BMI of 79.6kg and 26.1, respectively. In 2 cases the usual lateral and inferior hiper-reduction were also performed, and in the last case only the inferior resection. The average AST/ALT levels at POD1 were 130.5g/L and 145g/L, respectively, 130g/L and 196g/L at POD2. Donors were discharged at an average of 3.3 days, all operations were open surgery. The median recipients’age and BW at transplantation were 3.4 months and 4.3kg, respectively. The causes of liver disease were cryptogenic cirrhosis (2), and Alagille Sd (1). The median PELD score was 33, and 2 patients presented ascites at transplantation. The average PRBC transfusion was 21.3 ml/kg, and the median GRWR was 4.76, after the reductions. The values of each resected area of the LLS, as well as the initial and final antero-posterior length are shown in Table 1. The average percentage reduction in graft weight was 29.6%, and the average reduction in antero-posterior length was 35.4%. All patients were primarily closed and were extubated in the first post-operative day, and the average hospital stay was 26 days.
Conclusion: The anterior liver resection shown in this series was safe for donors and recipients. The observation of the anatomy of the left portal vein and its relation to the liver parenchyma and surface allowed the development of this simple and safe new technique for reducing the antero-posterior length of the liver.
Lectures by Joao Seda Neto
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Sun-26 13:45 - 14:45 |
Liver 1 | Outcome comparison between LDLT and DDT in a cohort of 840 pediatric recipients | Hill Country AB |
|
Tue-28 08:00 - 09:00 |
Surgery | Anterior hepatic resection: a simple and safe new technique for reducing the antero-posterior diameter of the liver graft for small pediatric recipients | Hill Country CD |
