Qiang Zhang, People's Republic of China
The First Affliated Hospital, Sun Yat-sen University
Single kidney transplantation using pediatric donor kidneys: satisfactory outcomes but specific attentions needed
Mingchuan Huang1, Wenrui Wu1, Xiaojun Su1, Jun Li1, Chenglin Wu1, Huanxi Zhang1, Qian Fu1, Jianming Li1, Shenghui Wu1, Yanxu Chen1, Qiang Zhang1, Longshan Liu1, Changxi Wang1.
1Department of Organ Transplant, The First Affiliated Hospital of Sun Yat-sen University, Guangzhou, People's Republic of China
Purpose: Utilization of pediatric donor in single kidney transplantation (SKT) are popular and can greatly expand the scarce donor pool, whereas potential risk factors remain unclear, which is crucial for improving post-transplant prognosis.
Methods: A total of 484 SKTs cases using pediatric donor kidneys performed in our center from Jan 2012 to Mar 2021 were retrospectively analyzed. Recipients were grouped by age: child (0-12y, n=143), adolescence (12-18y, n=86), adult (≥18y, n=255). The overall prognosis was analyzed and post-transplant outcomes between groups were compared and assessed by univariate and multivariate analysis using Cox proportional risk model.
Results: The average follow-up time was 30 months. 1- and 3-year patient survival was 98.7% and 96.8%, respectively. One-year and three-year death-censored graft survival (DCGS) were 96.1% and 92.7%, respectively. Overall eGFR at 1-year and 3-year are 80.0±24.5 and 84.2±25.2 mL/min/1.73 m2, and the 3-year eGFR of three groups were comparable and all were over 80 mL/min/1.73 m2, showing satisfactory graft function . Proteinuria decreased gradually within the six months post-transplant in all groups. Rejection was an independent risk factor of death-censored graft failure within three years after transplantation (HR=3.64, P=0.002). Further subgroup analysis showed that surgical-related complications are more common in child group than adult group (P=0.027), suggesting that surgical-related complications may associate with graft failure in child recipients in 0-30 days post-transplant.
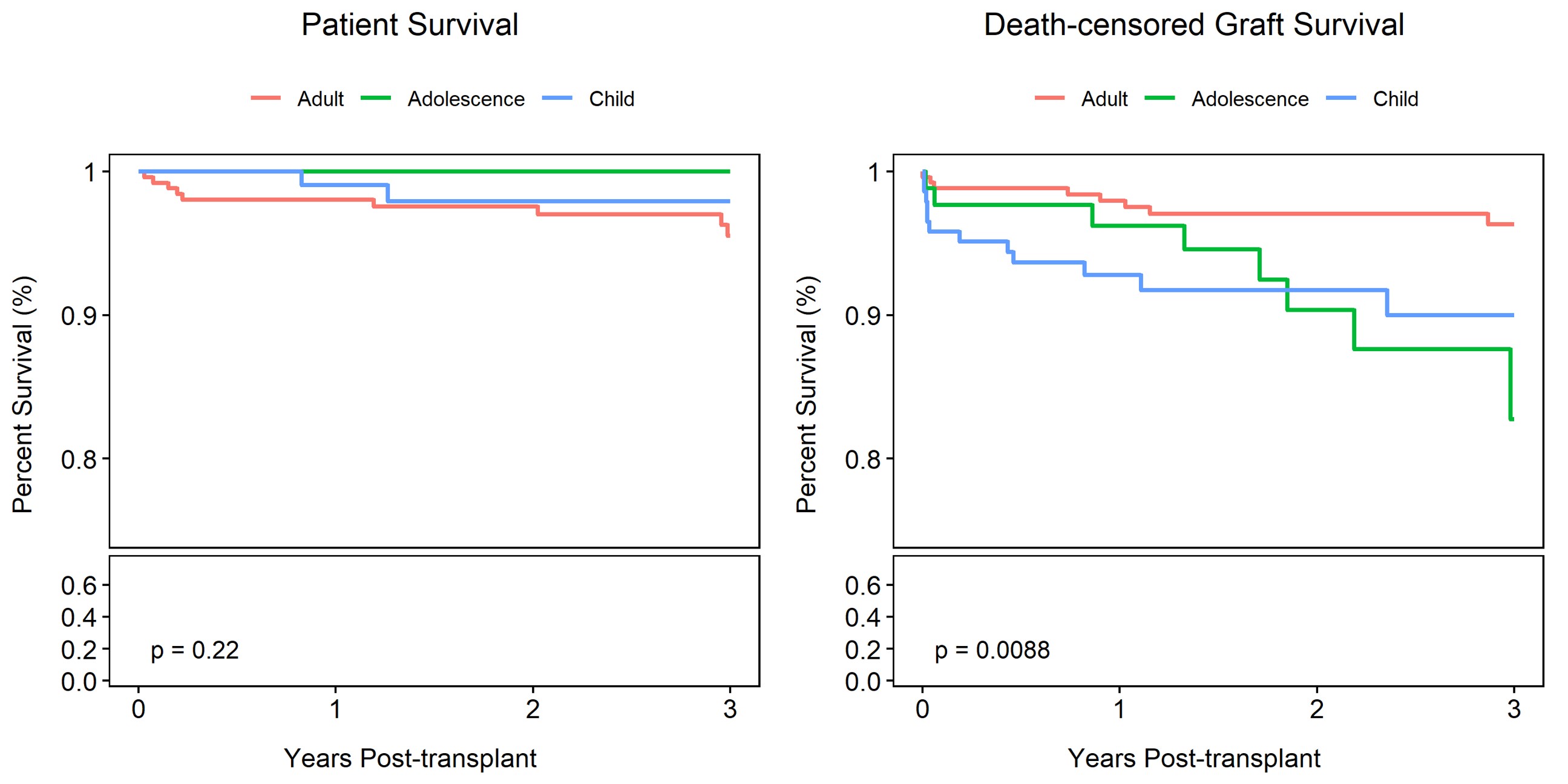
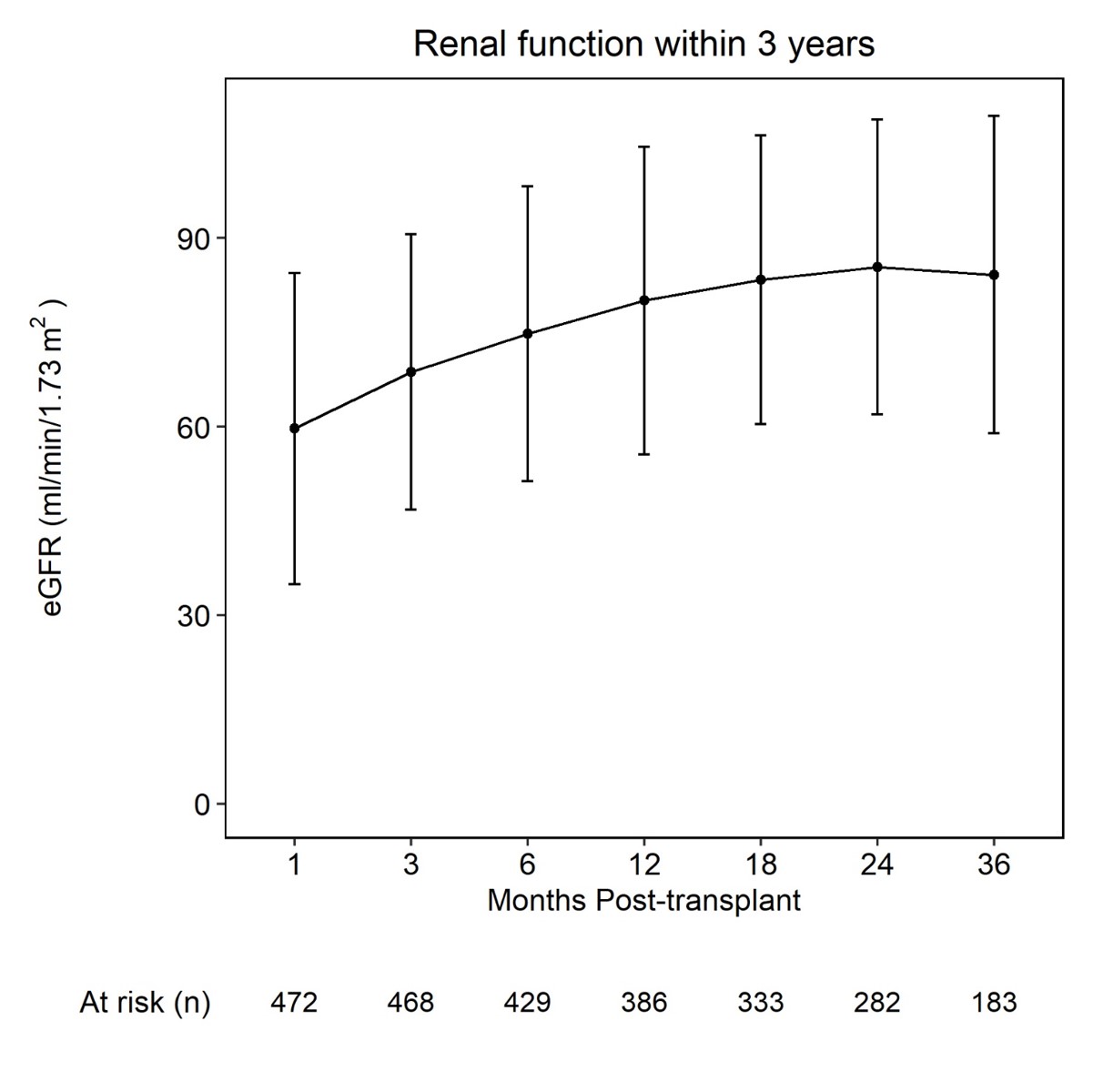
Conclusions: Single pediatric donor kidney transplantations could achieve decent outcomes while it should be noted that rejections were persistent obstacles in the early-middle post-transplant stage. In addition, child recipients may compromise their early postoperative outcomes for surgical-related complications. This study indicated risk factors in different recipient ages at different post-transplant time periods, suggesting that specific attentions should be paid to different patients at different time in order to ensure the post-transplant outcomes.
References:
[1] Hart A, Lentine KL, Smith JM, Miller JM, Skeans MA, Prentice M, et al. OPTN/SRTR 2019 Annual Data Report: Kidney. Am J Transplant. 2021;21 Suppl 2:21-137.
[2] Su X, Shang W, Liu L, Li J, Fu Q, Feng Y, et al. Transplantation of a single kidney from pediatric donors less than 10 kg to children with poor access to transplantation: a two-year outcome analysis. BMC Nephrol. 2020;21(1):250.
[3] Chen C, Su X, Wu C, Liu L, Zhang H, Deng R, et al. Successful single kidney transplantation from pediatric donors less than or equal to 10 kg to adult recipient: a retrospective cohort study. Transl Pediatr. 2021;10(6):1618-29.
[4] Zhu L, Fu C, Chen S, Liu B, Du D, Chang S, et al. Successful Single-kidney Transplantation in Adult Recipients Using Pediatric Donors Aged 8 to 36 Months: Comparable Outcomes With Those Using Pediatric Donors Aged >3 Years. Transplantation.. 2019;103(11):2388-96.
[5] Beetz O, Weigle CA, Nogly R, Klempnauer J, Pape L, Richter N, et al. Surgical complications in pediatric kidney transplantation-Incidence, risk factors, and effects on graft survival: A retrospective single-center study. Pediatr Transplant. 2021;25(2):e13871.
[6] Kabore R, Couchoud C, Macher MA, Salomon R, Ranchin B, Lahoche A, et al. Age-Dependent Risk of Graft Failure in Young Kidney Transplant Recipients. Transplantation. 2017;101(6):1327-35.
[7] Rianthavorn P, Ettenger RB. Medication non-adherence in the adolescent renal transplant recipient: a clinician's viewpoint. Pediatr Transplant. 2005;9(3):398-407.
[8] Sundaram SS, Landgraf JM, Neighbors K, Cohn RA, Alonso EM. Adolescent health-related quality of life following liver and kidney transplantation. Am J Transplant. 2007;7(4):982-9.
[9] Pelletier SJ, Guidinger MK, Merion RM, Englesbe MJ, Wolfe RA, Magee JC, et al. Recovery and utilization of deceased donor kidneys from small pediatric donors. Am J Transplant. 2006;6(7):1646-52.
Lectures by Qiang Zhang
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Mon-27 10:00 - 11:00 |
Kidney 3 | Utilization of Kidneys from Pediatric Donors with Acute Kidney Injury into Pediatric Kidney Transplant Recipients: A Single-center Experience | Zilker 3-4 |
|
Tue-28 09:10 - 10:10 |
Kidney | Single kidney transplantation using pediatric donor kidneys: satisfactory outcomes but specific attentions needed | Zilker 3-4 |
