Mohammad Fardeen Maudarbaccus, Canada
Clinical Fellow Pediatric Anesthesia
Pediatric Anesthesia
The Hospital for Sick Children, Toronto
Predictors of early extubation after pediatric liver transplant
Mohammad Fardeen Maudarbaccus1,2, Blayne A. Sayed3, Vicky Ng4, Elaine Gilfoyle5, Asad Siddiqui1,2.
1Pediatric Anesthesia, The Hospital for Sick Children, Toronto, ON, Canada; 2Department of Anesthesiology and Pain Medicine, University of Toronto, Toronto, ON, Canada; 3Division of General and Thoracic Surgery, The Hospital for Sick Children, Toronto, ON, Canada; 4Division of Gastroenterology, Hepatology, and Nutrition, The Hospital for Sick Children, Toronto, ON, Canada; 5Department of Pediatric Critical Care Medicine, The Hospital for Sick Children, Toronto, ON, Canada
Introduction: Liver transplantation is the life-saving treatment for many end-stage pediatric liver diseases with significant perioperative physiologic derangements. Despite this, early extubation after surgery has been proposed in small studies with a positive safety signal and potential for improved outcomes.1-3 The purpose of our study was to investigate the rate of extubation immediately after surgery in the operating room (OR) at a single high-frequency transplant institution, to delineate outcomes and identify predictors of early extubation.
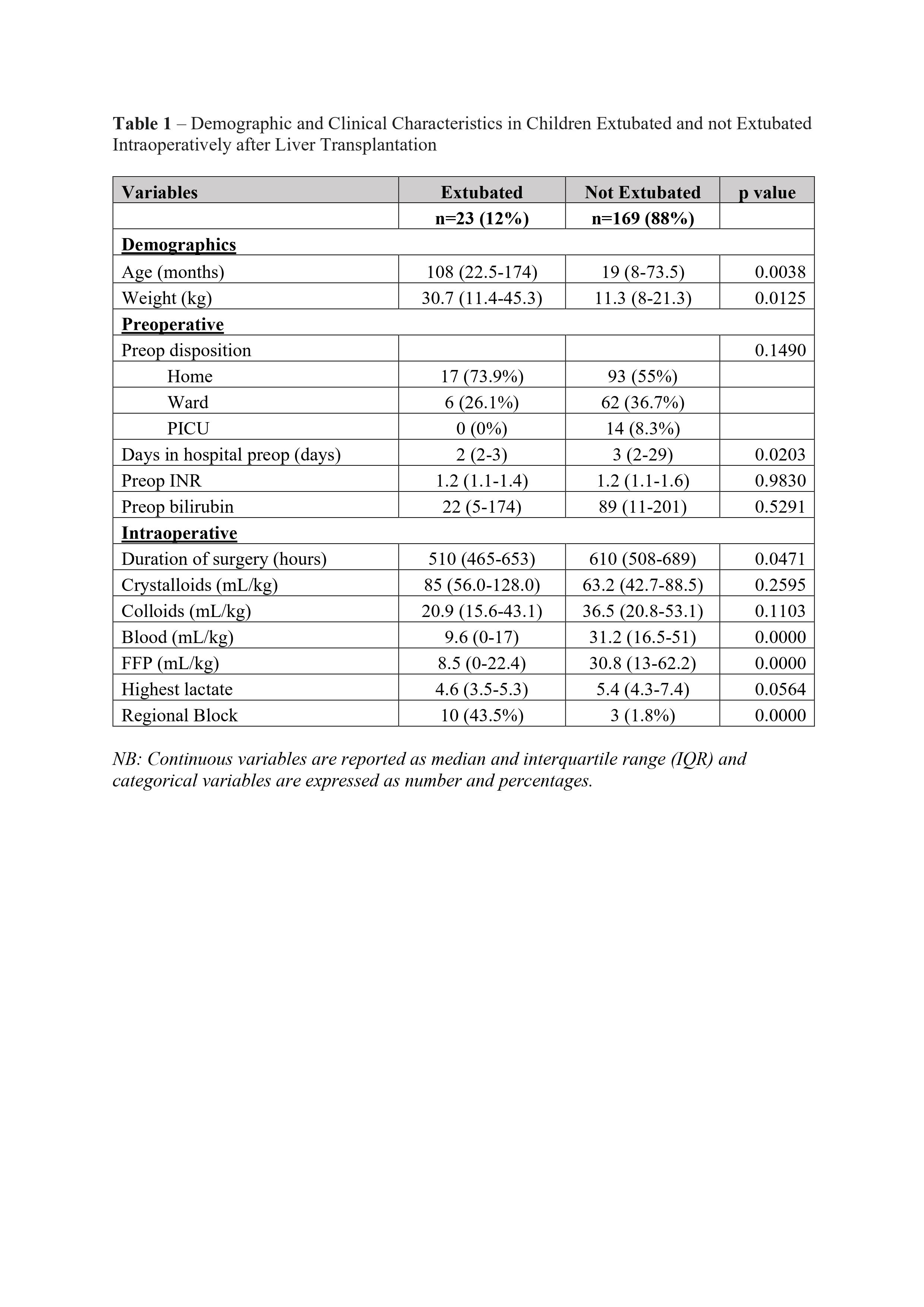
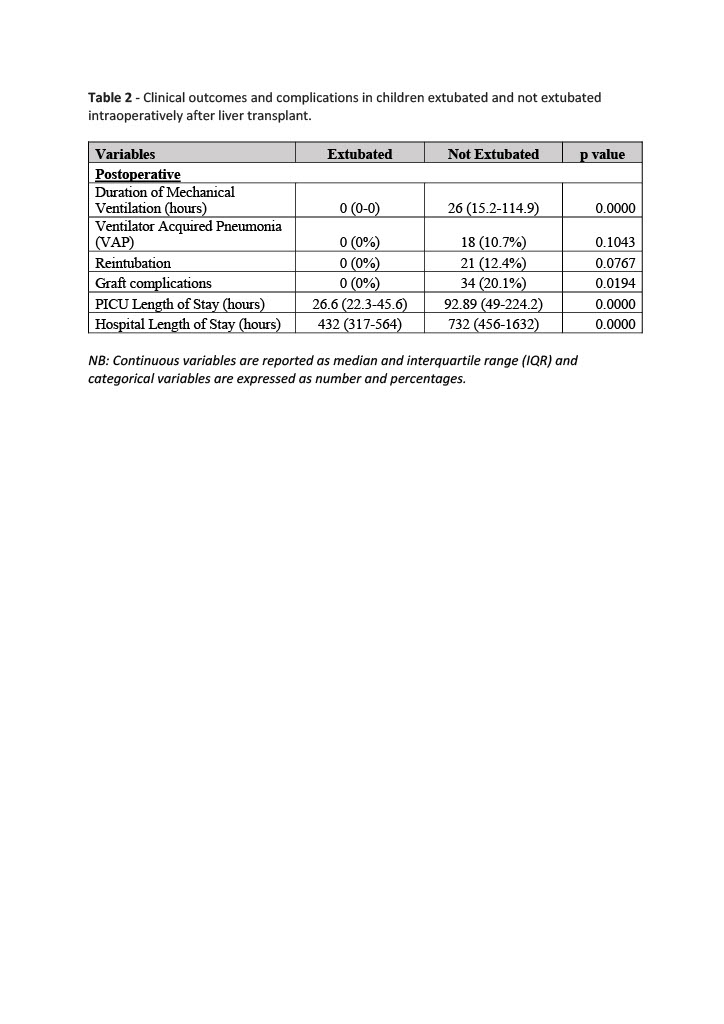
Methods: After obtaining ethics approval, the records of 192 children who underwent liver transplantation between 2013 to 2020 were retrospectively analysed. We classified the patients in two groups; those who were extubated in the OR immediately after surgery and those who remained intubated in the intensive care unit (ICU). We recorded multiple pre-operative, intra-operative and post-operative variables. (Table 1,2) We used student t-test to analyse continuous data and Chi square test to analyse categorical data. A p-value of < 0.05 was considered significant.
Results: All patients that underwent liver transplant between 2013 and 2020 were included in the study. 23/192 children (12%) were extubated intra-operatively. 82.6% of those extubated underwent liver transplant after 2017. Younger patients were more likely to remain intubated (p=0.038). There was no statistical difference between the 2 groups in regards to: preoperative disposition, preoperative INR and bilirubin, quantity of crystalloid or colloid administered and peak lactate. Criteria which were statistically significant for successful extubation included: older age, shorter length of stay (LOS) in hospital preoperatively, shorter duration of surgery, less red blood cell (pRBC) and fresh frozen plasma (FFP) transfusion and the presence of regional anesthesia (Table 1). None of the patients who were extubated had to be reintubated in the ICU. Our data also demonstrates that the early extubation group had a shorter ICU LOS, shorter hospital LOS, and less graft complications. Furthermore, the non-extubation group had a ventilator induced pneumonia (VAP) rate of 10.7% and reintubation rate of 12.4%. (Table 2)
Conclusion: Our data demonstrates that 12% of patients were extubated immediately after transplant in the OR and did not require reintubation in the ICU; however, 82.6% of these occurred after 2017 indicating a temporal trend towards extubation in more recent years. Pre-operative and intra-operative predictors of extubation included shorter LOS in hospital prior to transplant, older age, shorter length of surgery, smaller volume of pRBC and FFP transfused and utilization of regional anesthesia. Furthermore, the extubation group demonstrated a favourable clinical profile with decreased ICU and hospital LOS. These parameters can potentially guide decision making towards predicting early extubation candidates after pediatric liver transplantation.
References:
[1] Immediate extubation of children following liver transplantation is safe and may be beneficial. Transplantation80(7), 959-963. 2005
[2] Immediate Tracheal Extubation of Pediatric Liver Transplant Recipients in the Operating Room. Pediatr Transplantation 2003;7:381-384
[3] Immediate Tracheal Extubation After Liver Transplantation: Experience of Two Transplants Centers. Anesth Analg 1997;84:249-53.
Lectures by Mohammad Fardeen Maudarbaccus
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Sat-25 18:00 - 19:15 |
P7- Liver / Intestine Posters | Predictors of early extubation after pediatric liver transplant | Zilker 1-2 |
