Mats Steffi Jennifer Masilamani, United States
Pediatric Cardiology Fellow
Pediatric Cardiology
Mayo Clinic
Transcatheter Pulmonary Flow Restrictors as a Palliative Bridge to Transplant
Mats Steffi Jennifer Masilamani1, Jason H. Anderson1, Allison K. Cabalka1, Nathan W. Taggart1, Rebecca K. Ameduri1, Joseph A. Dearani1, Elizabeth H. Stephens1, Jonathan N. Johnson1.
1Pediatric Cardiology, Mayo Clinic, Rochester, MN, United States
Background: Transcatheter implantation of devices restricting branch pulmonary arterial flow has been reported as a potential alternative to traditional surgical pulmonary artery banding.
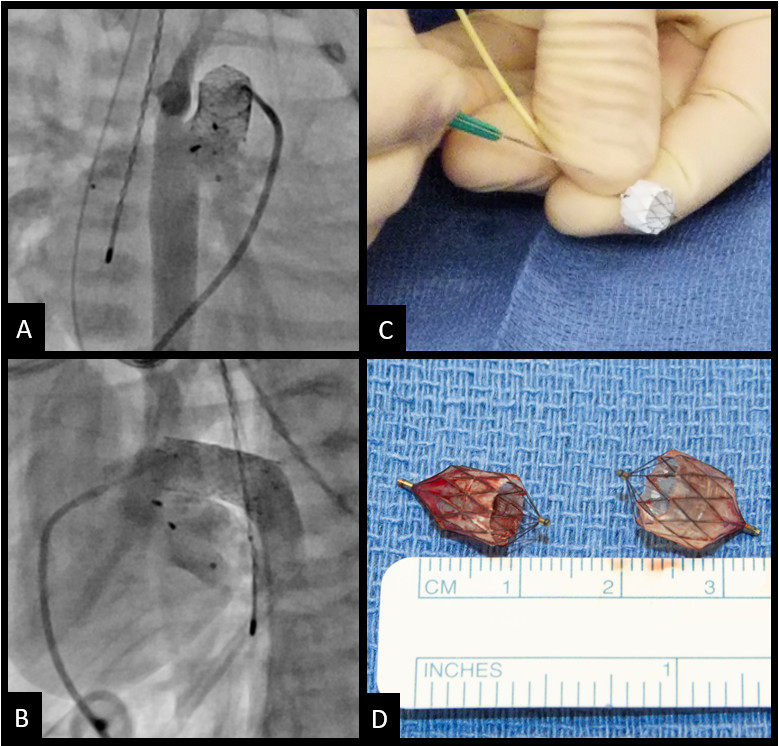
Case presentation: A term male was diagnosed postnatally with critical aortic stenosis and reduced ejection fraction of 10-15%. He underwent aortic balloon valvuloplasty on day of life 2, which immediately improved forward flow. However, he continued to have a severely dilated left ventricle with severely reduced ejection fraction of 15%. He remained ductal dependent for systemic perfusion requiring prostaglandin for ductal patency. He also had increasing overcirculation. On day of life 14, he underwent a palliative catheter procedure including placement of bilateral pulmonary flow restrictors (PFRs) (fenestrated Medtronic Micro Vascular Plug (MVP) 7Q devices), and stenting of the ductus with a 8 mm diameter ev3 Visi-Pro stent. He improved clinically after this procedure with resolution of his overcirculation. He weaned off respiratory support and was taking oral feeds while awaiting transplant. Twelve days after the procedure, a donor heart became available, and he underwent cardiac transplantation. The transplantation and recovery were uneventful. At latest follow-up 15 months post-transplant, he is doing well and growing as expected for age.
Conclusion: A catheterization-based approach to palliation using endoluminal pulmonary arterial flow restriction was helpful in stabilization of the infant and successfully bridged him to transplant. This strategy could be used for other patients with ductal dependent lesions with pulmonary overcirculation awaiting transplantation or other surgical repairs.
References:
[1] Singh GK. Congenital Aortic Valve Stenosis. Children (Basel). 2019 May 13;6(5):69. doi: 10.3390/children6050069. PMID: 31086112; PMCID: PMC6560383.
[2] Schranz D, Esmaeili A, Akintuerk H. Hypoplastic Left Heart: Stage-I Will be Performed Interventionally, Soon. Pediatr Cardiol. 2021 Apr;42(4):727-735. doi: 10.1007/s00246-021-02597-y. Epub 2021 Apr 19. PMID: 33871681; PMCID: PMC8110497.
Lectures by Mats Steffi Jennifer Masilamani
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Sat-25 18:00 - 19:15 |
P9- Thoracic Posters | Transcatheter Pulmonary Flow Restrictors as a Palliative Bridge to Transplant | Zilker 1-2 |
