Ioannis A. Ziogas, United States
General Surgery Resident
Department of Surgery
University of Colorado Anschutz Medical Campus
Pediatric Liver Transplantation for Hepatoblastoma According to Graft Type
Ioannis Ziogas1,2, Nicholas Schmoke1,2, Dor Yoeli1,2, Jonathan M. Cullen1,2, Julia M. Boster3, Michael E. Wachs1,2, Megan A. Adams1,2.
1Division of Abdominal Transplant Surgery, Department of Surgery, Children's Hospital Colorado, University of Colorado, Anschutz Medical Campus, Aurora, CO, United States; 2Colorado Center for Transplantation Care, Research and Education (CCTCARE), Department of Surgery, University of Colorado School of Medicine, Aurora, CO, United States; 3Department of Pediatrics, Section of Pediatric Gastroenterology, Hepatology & Nutrition, Children's Hospital Colorado, University of Colorado, Anschutz Medical Campus, Aurora, CO, United States
Introduction: Liver transplantation (LT) is the only potentially curative option for children with unresectable hepatoblastoma. Although post-transplant outcomes have improved in the contemporary era, the effect of donor graft type on survival is unclear.
Methods: We compared the demographics, clinical characteristics, and survival after first isolated LT for hepatoblastoma in children (<18 years) according to donor graft type using United Network for Organ Sharing data (02/2002-06/2021). Kaplan-Meier method, log-rank tests, and Cox regression modelling were used to evaluate the effect of whole, partial, and split deceased donor liver transplant (DDLT) and living donor liver transplant (LDLT) on patient and graft survival.
Results: A total of 590 pediatric hepatoblastoma LT recipients (344 whole graft DDLT; 62 partial graft DDLT; 139 split graft DDLT; 45 LDLT) were included. The median age for the cohort was 2 years and the median weight was 11.9 kg. There were no significant differences in demographics among the four groups except for the fact that partial graft DDLT recipients were larger compared to the rest (P=0.03). Median waitlist time was 26 days for the cohort and was not different among the four graft type groups (P=0.29). During 2002-2021, 72.5% of the patients had received a status 1B exception, while that percentage was 97.3% after the automatic 1B exception implemented in 2012. The 5-year post-transplant patient and graft survival rates for the entire cohort were 82.4% and 76.5%, respectively, while no differences were identified among the four groups regarding patient (P=0.45; Fig.A) or graft survival (P=0.69; Fig.B).
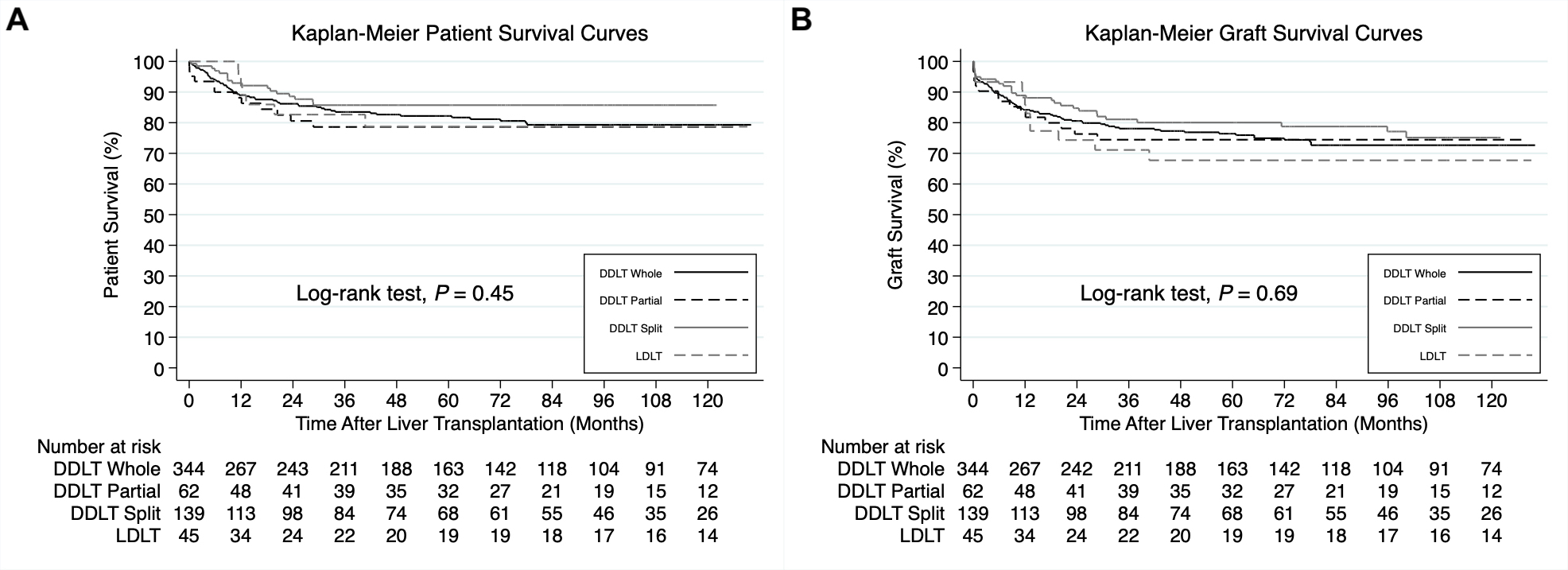
The results remained similar during the 2002-2011 era, while during the 2012-2021 era, split graft DDLT was associated with decreased graft loss risk when compared to whole graft DDLT (P=0.046) without any other significant between-group differences.
Conclusion: Survival outcomes after pediatric LT for hepatoblastoma appear to be favorable, while non-whole grafts demonstrate equal if not better outcomes. LDLT allows for timing of transplant around neoadjuvant chemotherapy and may help reduce the burden of unnecessary chemotherapy cycles, while children wait for a deceased donor graft. However, LDLT seems to be an underutilized resource for hepatoblastoma (7.6% of all LTs). Thus, future efforts should focus on expanding the donor pool through LDLT (e.g., non-directed) to optimize multidisciplinary oncologic treatment for hepatoblastoma and improve survival while decreasing waiting list mortality.
Lectures by Ioannis A. Ziogas
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Sat-25 17:00 - 18:00 |
Liver / Intestine | Pediatric Liver Transplantation for Hepatoblastoma According to Graft Type | Zilker 3-4 |
