Orthotopic heart transplantation in pediatric Marfan syndrome patients: A review of the Pediatric Health Information System database
Stephanie S. Philip1,3, Sruthi Ilangovan1,3, Andrew Well2,3, Matthew F. Mikulski2,3, Carlos M. Mery2,3, Lauren D. Glass1,3, Chesney D. Castleberry1,3.
1Department of Pediatrics, Dell Medical School at The University of Texas at Austin, Austin, TX, United States; 2Department of Surgery and Perioperative Care, Dell Medical School at The University of Texas at Austin, Austin, TX, United States; 3Texas Center for Pediatric and Congenital Heart Disease, Dell Medical School at The University of Texas at Austin, Austin, TX, United States
Introduction: Marfan Syndrome (MFS) is an autosomal dominant connective tissue disorder that conveys substantial aortic and cardiovascular morbidity. MFS patients often develop refractory heart failure; however, the recommendation for orthotopic heart transplant (OHT) for this population is considered controversial given the potential for progression of aortic and cardiovascular complications. Outcomes post-transplant for MFS patients are not well-described.
Methods: A retrospective review of the Pediatric Health Information System (PHIS) was performed. All encounters <18 years of age between 1/1/2004 – 6/30/2022 with a diagnosis code for MFS were identified. MFS encounters with an OHT procedure code were isolated, and all encounters (pre- and post-OHT) for those patients were evaluated. Diagnoses and procedures were identified utilizing the International Classification of Diseases, 9th and 10th revisions. Demographics, diagnoses, and outcomes were identified and analyzed using descriptive statistics.
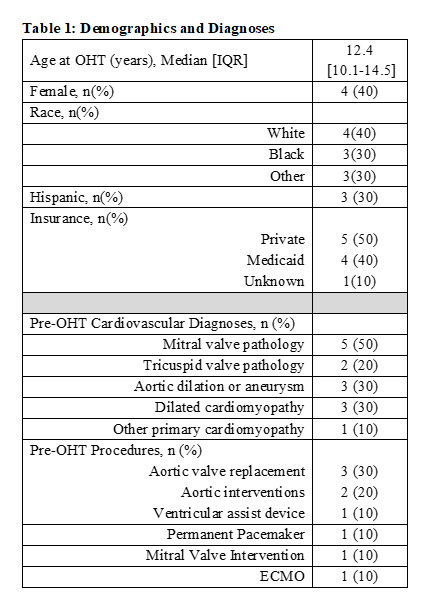
Results: A total of 10 eligible MFS patients were identified out of 5438 linked-encountered MFS patients in the PHIS database. Of those, 4 (40%) were female, 4 (40%) were White, 3 (30%) were Hispanic, and 5 (50%) had private insurance. The median age at OHT was 12.4 [IQR: 10.0 – 14.5] years. (Table 1).
Prior to OHT, five (50%) had mitral valve and two (20%) had tricuspid valve pathologies. Three (30%) patients had a diagnosis of dilated cardiomyopathy and an additional patient (10%) had a diagnosis of “other primary cardiomyopathy.” Three (30%) had aortic dilation or aneurysm. Pre-OHT, three (30%) patients had an aortic valve replacement, 2 (20%) had aortic interventions and 1 (10%) received a durable implantable ventricular assist device (VAD).
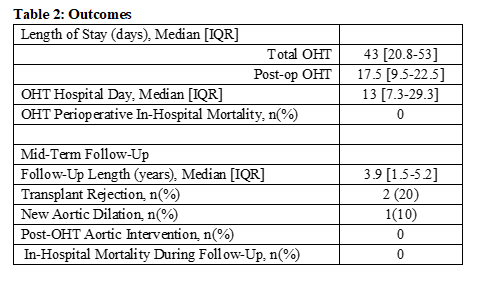
Median post-OHT length of stay was 17.5 [IQR: 9.5-22.5] days. One (10%) patient was supported with extracorporeal membrane oxygenation (ECMO) immediately prior to transplant. There were no perioperative mortalities following OHT. However, one (10%) patient did require post-OHT ECMO with an eventual transition to a VAD.
Over a median follow-up of 3.9 [IQR: 1.5-5.2] years, there were no in-hospital mortalities and no repeat transplants. Additionally, no patients were noted to have a diagnosis of coronary disease or underwent aortic intervention. However, two (20%) were noted to have a diagnosis of transplant rejection (Table 2).
Conclusion: Pediatric MFS patients rarely receive cardiac transplantation. However, this small cohort demonstrates 100% perioperative survival without any known MFS-related cardiovascular interventions post-OHT. Further research is needed to understand the long-term outcomes of MFS patients who undergo OHT to determine if MFS confers added risk.
References:
[1] Knosalla C, Weng Y, Hammerschmidt R et al. Orthotopic Heart Transplantation in Patients with Marfan Syndrome. Ann Thorac Surg. 2007;83(5):1691-1695.
[2] Murdoch JL, Walker BA, Halpern BL, Kuzma JW, McKusick VA. Life Expectancy and Causes of Death in the Marfan Syndrome. N Engl J Med. 2010;286(15):804-808.
Lectures by Stephanie S. Philip
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Sat-25 17:00 - 18:00 |
Thoracic (Heart) | Orthotopic heart transplantation in pediatric Marfan syndrome patients: A review of the Pediatric Health Information System database | Hill Country CD |
