Adewale Elijah Adetunji, South Africa
Paediatric Renal Fellow
Paediatric
Red Cross War Memorial Children Hospital
Evaluation of the implementation of a ‘paediatric feasibility assessment for transplantation’ (pFAT) form in children and adolescents at Red Cross War Memorial Children’s Hospital (RCWMCH), Cape Town, SA
Adewale Adetunji1, Priya Gajjar1, Valerie Luyckx1, Deveshni Reddy1, Peter Nourse1, Ashton Coetzee1, Nicole Collison1, Theresa Abdo1, Taryn Pienaar1, Christel Du Buisson2, Jonathan Buckley1, Brenda Morrow1, Mignon McCulloch1.
1Paediatric Nephrology, Red Cross War Memorial Children's Hospital, Cape Town, South Africa; 2Paediatric Nephrology, Tygerberg Hospital, Cape Town, South Africa
Introduction: Kidney transplantation, remains the treatment of choice for children with ESKD [1, 2], however success of pediatric transplantation depends on many factors. Kidneys are a scarce resource and should be allocated to those where success is likely [3]. Predicting success however is challenging. Experience of challenging cases with poor outcomes led to the development of the ‘Paediatric Feasibility Assessment for Transplantation’ (pFAT) form at RCWMCH in Cape Town, after critical evaluation of graft and patient survival over three decades. A more objective and transparent system with which to list patients for kidney transplantation was needed, to ensure consistency and equity in patient selection, and reduce moral distress among clinicians [4].
Objective: Evaluation of implementation of the (pFAT) form in all children evaluated for dialysis/kidney transplantation to identify factors most associated with listing/non-listing for transplantation, and to assess outcomes among those listed for transplantation
Methods: Anonymized data was extracted from the Paediatric Nephrology database of all patients <18years evaluated for dialysis/transplantation with the pFAT form at RCWMCH from 2015 – 2021.
Results: 88 children were assessed using pFAT, 58 (65.9%) of whom were listed for dialysis/kidney transplant. Table 1 shows characteristics of the patients assessed.
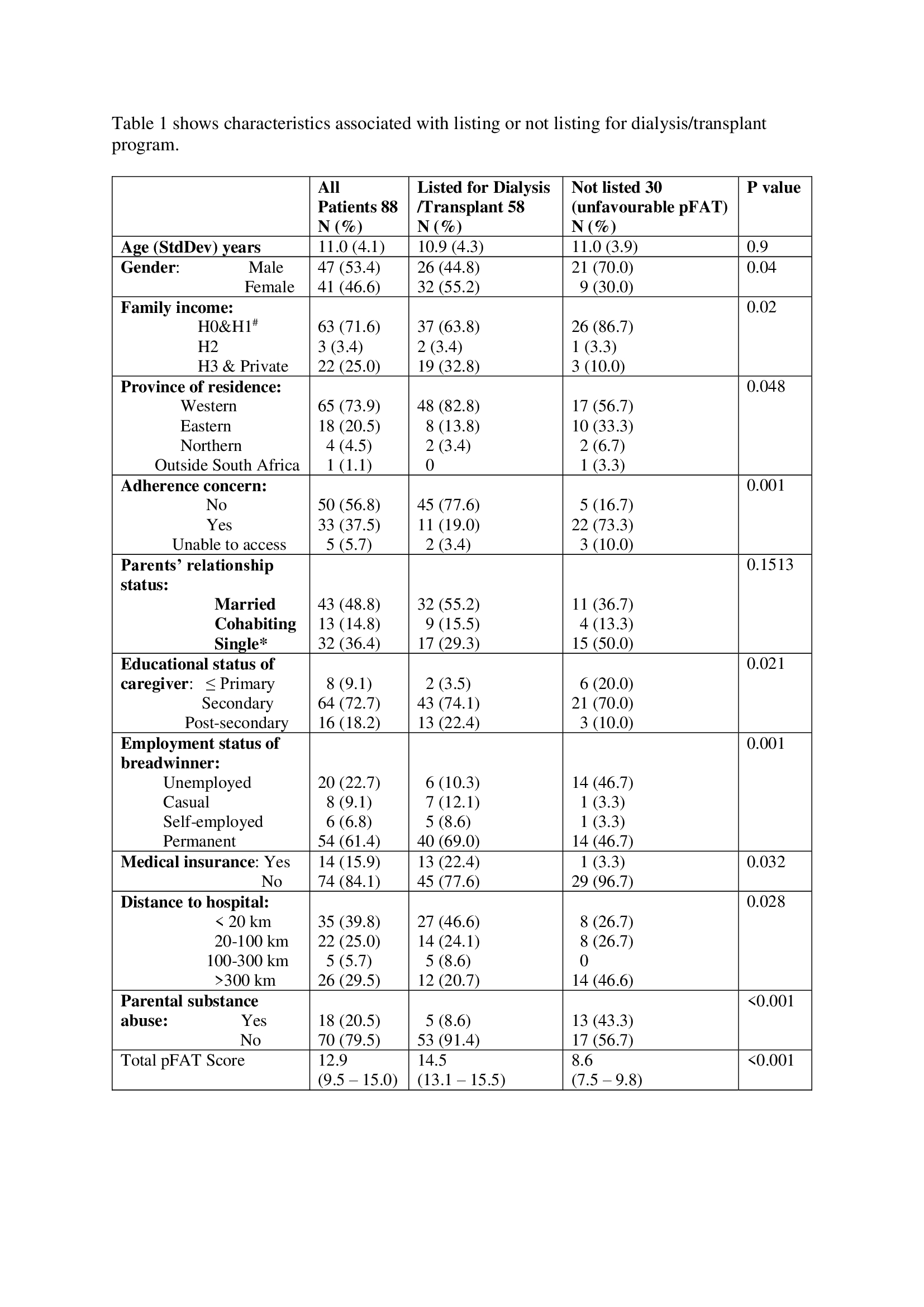
Children not listed scored very low in social support, adherence, and caregiver concerns. Overall, a pFAT score of over 13/16 was associated with an acceptable 1-year graft survival.
Forty children been transplanted, 32 have completed 1 year follow-up.
Despite low 1 year graft survival of 84.4%(27/32) due to medical issues (2 graft vascular thrombosis, 1 Covid-19, 1 nephrotic recurrence, 1 acute rejection) no grafts were lost due to psychosocial issues. Of the children not listed, 46.7% (14/30) of children died of which 10 were within a year of assessment.
Conclusions: The pFAT form was useful in objectively assessing family and patient characteristics, facilitating a transparent evaluation process. The form clearly highlights factors most frequently leading to non-listing for dialysis/transplantation. This emphasises the urgent need to implement psychosocial support to address remediable factors such as adherence, to address socio-economic barriers such as poverty, medical insurance, and to provide more comprehensive social support. Among those transplanted, no grafts were lost due to psychosocial issues suggesting the current form is associated with successful transplantation. Future work is required to validate the utility of the form in independent populations under similar resource circumstances, and to refine the weights attributed to the various components of the score.
References:
[1] McDonald SP, Craig JC. Long-term survival of children with end-stage renal disease. N Engl J Med. 2004;350 :2654-62.
[2] Fadare JO, Salako BL. Ethical issues in kidney transplantation–reflections from Nigeria. Transplant Research and Risk Management. 2010;2:87-91
[3] Batabyal P, Chapman JR, Wong G, Craig JC, Tong A. Clinical practice guidelines on wait-listing for kidney transplantation: consistent and equitable? Transplantation. 2012;94:703-13.
[4] Giacomini MK, Cook DJ, Streiner DL, Anand SS. Using practice guidelines to allocate medical technologies: an ethics framework. International Journal of Technology Assessment in Health Care. 2000;16:987-1002.
Lectures by Adewale Elijah Adetunji
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Sun-26 10:00 - 11:00 |
Ethical/Psychosocial and Economical Issues | Evaluation of the implementation of a ‘paediatric feasibility assessment for transplantation’ (pFAT) form in children and adolescents at Red Cross War Memorial Children’s Hospital (RCWMCH), Cape Town, SA | Hill Country CD |
