Validation of a dynamic prediction model of kidney allograft survival in pediatric kidney transplant recipients
Geeta Karadkhele1, Florian Manca2, Rémi Kabore3, Rachel Patzer1, Jérôme Harambat3,4, Karen Leffondre3, Julien Hogan1,2,5.
1Emory Transplant Center, Department of Surgery, Emory School of medicine, Atlanta, GA, United States; 2Pediatric nephrology department, Robert Debre Hospital, APHP, Paris, France; 3INSERM, Bordeaux Population Health Research Center, UMR1219, University of Bordeaux, Bordeaux, France; 4Pediatric nephrology Unit, Pellegrin Children Hospital, Bordeaux University Hospital, Bordeaux, France; 5Paris Translational Research Center for Organ Transplantation, INSERM, UMR-S970, Université Paris Cité, Paris, France
Introduction: Accurate prediction models of kidney allograft loss are lacking in children. Dynamic models allow the integration of new data throughout a patient’s follow-up making them better fitted from clinical use than traditional predictive models. In this study, we aim at externally validating a dynamic score of kidney allograft loss, developed in a derivation cohort of 793 French pediatric kidney transplant recipients, in a large cohort from the United States.
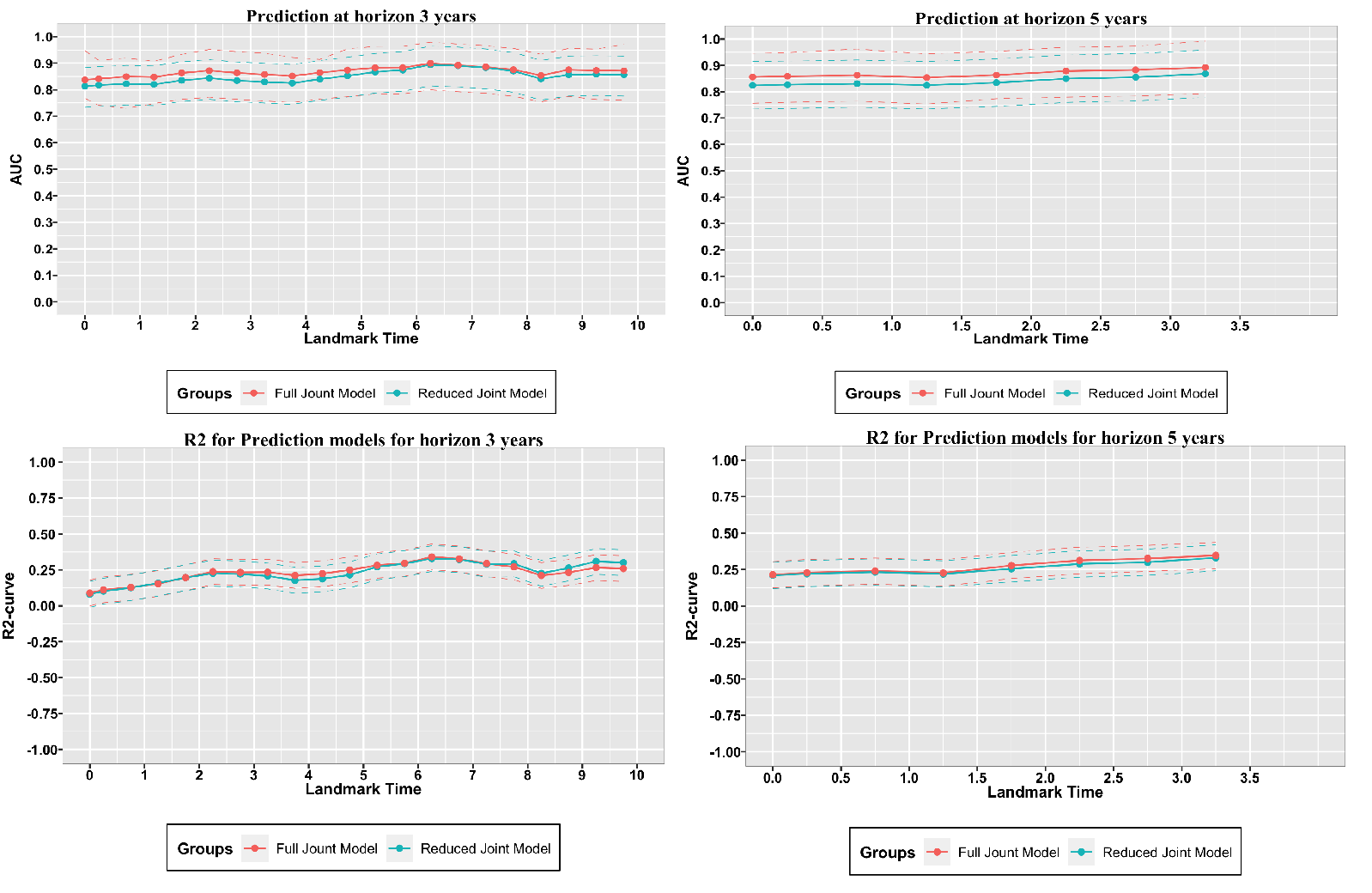
Methods: All patients aged < 21 years old, transplanted in the US between January 1st 2002 and December 31st 2015 recorded in the SRTR registry were included in the validation cohort. Two predictive models were previously developed using joint models on the French National Registry data (REIN) and included recipient, donor and transplant characteristics and follow-up data (eGFR, eGFR slope). Individual predictions of allograft loss at 3 and 5 years were made by applying these two models on the validation cohort. Model accuracy was evaluated based on its discrimination (AUC) and calibration (R2).
Results: 10,613 patients were included. Among them, 94% were younger than 18 years old at the time of transplantation, 59% were male, 28% received a preemptive transplant and 43% a living donor transplant. Over a median follow-up time of 6.6 [4.0;9.7] years, 2420 patients (23%) lost their graft and 316 (6%) died. The performances of the models were good with excellent discrimination (AUCs between 0.8 and 0.9) and good calibration (Figure 1). The performance of the reduced model were similar to those of the full model.
Conclusion: This predictive model demonstrated high accuracy in predicting kidney allograft loss in children and support the benefit of incorporating longitudinal information to improve prediction performance. This model can be used prospectively to assess patients’ risk of graft loss and further study evaluating the impact of using this model in clinical practice are needed.
Lectures by Julien Hogan
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Sun-26 13:45 - 14:45 |
Kidney 2 | Validation of a dynamic prediction model of kidney allograft survival in pediatric kidney transplant recipients | Zilker 3-4 |
|
Tue-28 10:40 - 11:40 |
Immunosuppression | Management of immunosuppression model-informed precision dosing | Hill Country CD |
