Pediatric Liver Transplant at Long-Distance High-Volume Centers Confers Improved Graft Survival Compared to Local Low-Volume Transplant Centers
Kliment Bozhilov1, Daniel Stotlz1, Andrew Bonham1, Varia Kirchner1, Grant Lum1, Carlos Esquivel1, Amy Gallo1.
1Department of Abdominal Transplant, Lucile Packard Children's Hospital at Stanford Universitry, Palo Alto, CA, United States
Introduction: Patient access to high-volume (HV) centers may be limited by resources and distance, which could ultimately negate the survival advantage conferred by HV centers. We investigated the difference in waitlist mortality, graft, and patient survival in patients that traveled greater than 100 miles to out of state (OS 100) HV centers compared to patients that received a liver transplant at local low-volume (LV) centers.
Methods: Pediatric patients undergoing liver transplant between 2010-2020 were identified using the SRTR database. Transplant centers were designated as HV or LV based on the average number of pediatric liver transplants performed per year (HV: ≥5 and LV: <5). Waitlist mortality, graft and patient survival for children receiving in-state transplants at a LV center were compared to patients undergoing out of state liver transplant at HV centers that were >100 miles from the state border using Kaplan-Meier curves and log-rank tests.
Results: Waitlist mortality was similar between patients receiving liver transplant at in state LV centers and HV OS100 centers (p = 0.24). However, graft survival was significantly better for children transplanted at HV OS100 centers compared to LV centers (p=0.00032, Figure 1). Overall patient survival between centers was not significantly different (p = 0.34) (Figure 2).
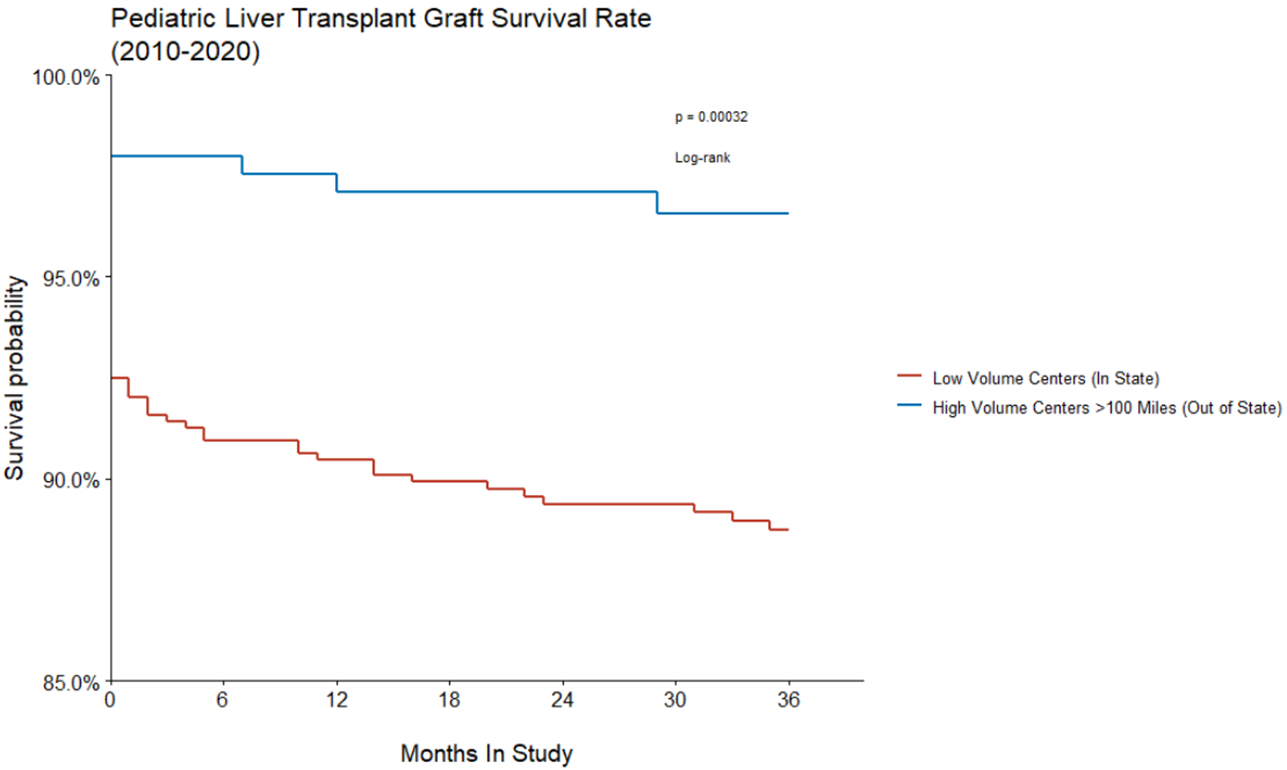
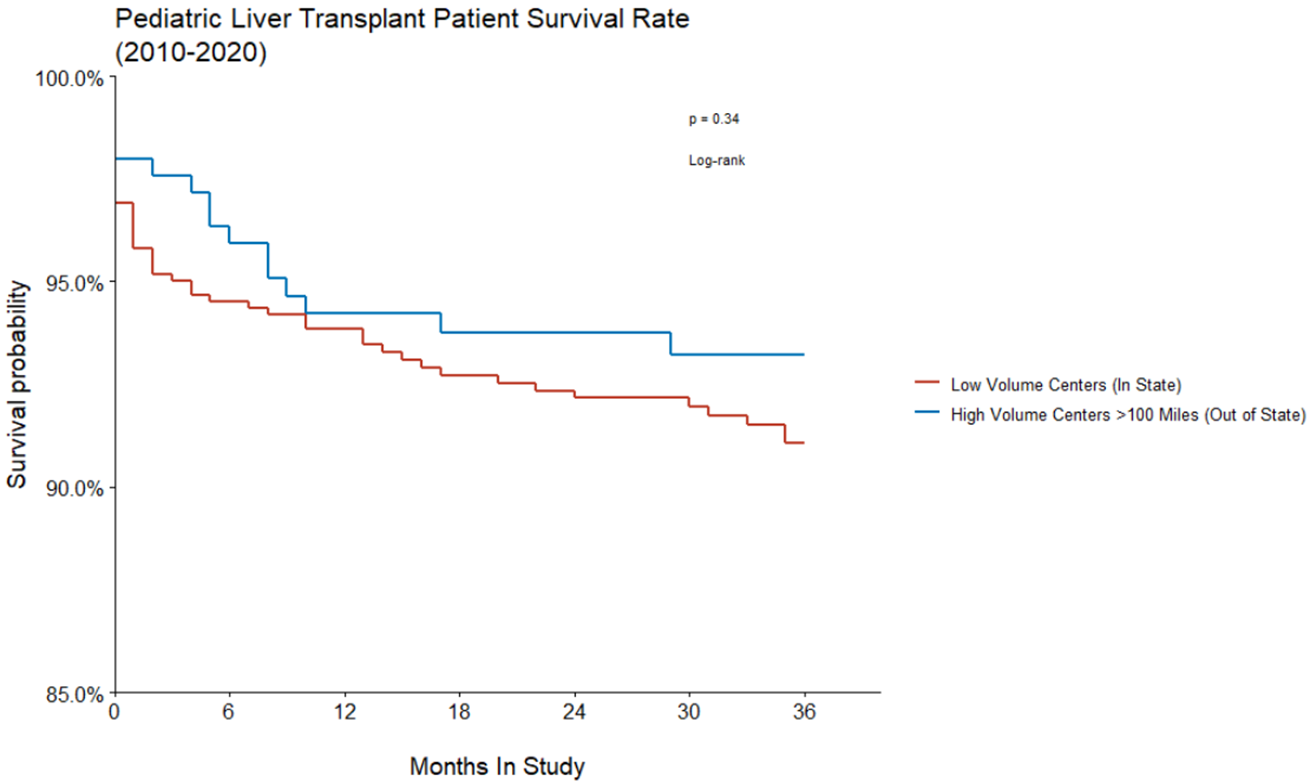
Conclusion: Patients that traveled >100 miles to receive an out of state liver transplant at HV centers had better graft survival than patients that received a liver transplant at local LV centers. There was no difference between the two groups with respect to waitlist mortality and overall survival. This suggests a higher retransplant rate at LV centers. Despite concerns for patient access to care due to distance, transplantation at HV centers may reduce the need for retransplant without increasing waitlist or overall mortality. More diligent monitoring by HV centers and collaboration with local LV centers is required to continue to improve access to care and outcomes for pediatric liver transplant recipients.
References:
[1] Nichols TJ, Price MB, Villarreal JA, Bakhtiyar SS, Vierling JM, Cotton R, Galvan T, O'Mahony CA, Goss JA, Rana A. Most pediatric transplant centers are low volume, adult-focused, and in proximity to higher volume pediatric centers. J Pediatr Surg . 2020 Aug;55(8):1667-1672. doi: 10.1016/j.jpedsurg.2019.10.019. Epub 2019 Nov 1. PMID: 31753609.
[2] Tracy ET, Bennett KM, Danko ME, Diesen DL, Westmoreland TJ, Kuo PC, Pappas TN, Rice HE, Scarborough JE. Low volume is associated with worse patient outcomes for pediatric liver transplant centers. J Pediatr Surg . 2010 Jan;45(1):108-13. doi: 10.1016/j.jpedsurg.2009.10.018. PMID: 20105589.
[3] Rana A, Pallister Z, Halazun K, Cotton R, Guiteau J, Nalty CC, O'Mahony CA, Goss JA. Pediatric Liver Transplant Center Volume and the Likelihood of Transplantation. Pediatrics . 2015 Jul;136(1):e99-e107. doi: 10.1542/peds.2014-3016. Epub 2015 Jun 15. PMID: 26077479.
[4] Adler JT, Bababekov YJ, Markmann JF, Chang DC, Yeh H. Distance is associated with mortality on the waitlist in pediatric liver transplantation. Pediatr Transplant . 2017 Mar;21(2). doi: 10.1111/petr.12842. Epub 2016 Nov 1. PMID: 27804189.
Lectures by Kliment Bozhilov
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Sun-26 13:45 - 14:45 |
Liver 1 | Pediatric Liver Transplant at Long-Distance High-Volume Centers Confers Improved Graft Survival Compared to Local Low-Volume Transplant Centers | Hill Country AB |
