Intraoperative continuous renal replacement therapy in critically ill pediatric liver transplant recipients; a case series
Louise K. Furukawa1, Olga N. Wolke1, Amy Gallo2, Scott Sutherland3, Julianne Mendoza1.
1Department of Anesthesia, Perioperative and Pain Medicine, Stanford University School of Medicine, Stanford, CA, United States; 2Department of Surgery, Stanford University School of Medicine, Stanford, CA, United States; 3Department of Pediatrics, Division of Nephrology, Stanford University School of Medicine, Stanford, CA, United States
Introduction: Pediatric patients in liver failure present challenges in the perioperative phase of liver transplantation. Coagulopathy, hypervolemia, oliguria, hyperkalemia and hyperammonemia are common and many patients require preoperative and/or intraoperative and postoperative continuous renal replacement therapy (CRRT). Although patient size, hemodynamic instability and vascular access present challenges to this modality, CRRT can prevent or mitigate hyperkalemia, acidosis, hyperammonemic encephalopathy, cerebral edema and volume overload that can occur during transplantation. We describe our institutional experience with intraoperative CRRT in our most critically ill pediatric liver transplant recipients.
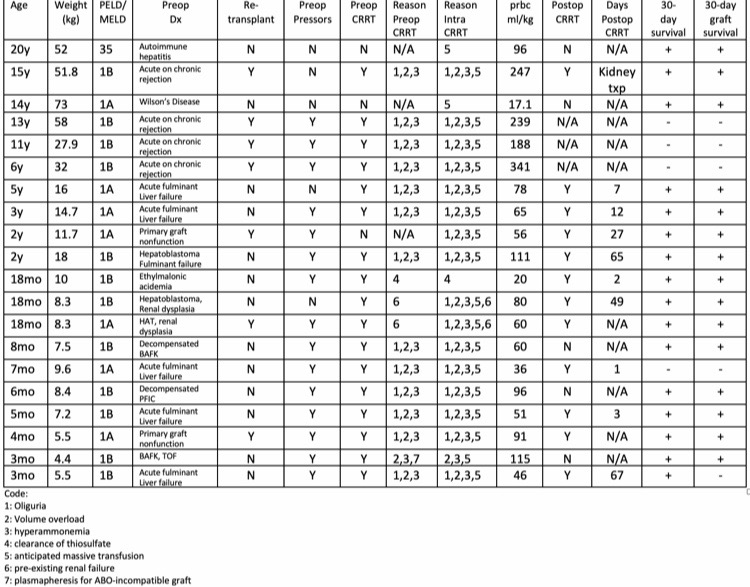
Methods: We conducted a five-year retrospective review (2015-2020) characterizing pediatric liver transplant recipients undergoing intraoperative CRRT during transplantation. We report preoperative diagnoses, liver disease severity, intraoperative transfusion requirement, need and duration of postoperative CRRT and perioperative patient and graft survival.
Results: 20 patients aged 3 months to 20 years underwent liver transplantation with intraoperative CRRT between 2015-2020. Median age was 21 months. 95% were listed status 1A or 1B. 35% were retransplants. 85% required preoperative CRRT. Reasons included hyperammonia and renal insufficiency in 67%. Other indications were pre-existing renal failure, preoperative thiosulfate clearance, and plasmapheresis. Perioperative mortality was 20%. Three intraoperative deaths were attributed to hemorrhage and one postoperative death resulted from primary graft nonfunction and hemorrhage. Thirty-day graft survival was 75%. Postoperative CRRT was required in 71% for a period of 1-67 days. Dialysis independence was achieved in 92% (11/12); one patient developed ESRD and required renal transplantation.
Conclusion: Much has been published on the use of intraoperative CRRT in adults during liver transplantation, but little has been documented in children (1). Pediatric patients are particularly prone to hyperkalemia and other electrolyte disturbances during massive transfusion and the metabolic consequences of liver transplantation, hemorrhage and reperfusion predisposes these patients to a higher risk of intraoperative critical events (2). Despite vascular access limitations, hemodynamic instability and coagulopathy, pediatric intraoperative CRRT can be a useful modality in the treatment of critically ill pediatric patients undergoing liver transplantation.
[1] Nadim M et al. Intraoperative hemodialysis during liver transplantation: a decade of experience Liver Transpl .2014;20:756-64
[2] Lee A et al. Transfusion-associated kyperkalemic cardiac arrest in pediatric patients receiving massive transfusion. Transfusion.2014;54:244-54