
A Systematic Review of Social Determinants of Health in Pediatric Organ Transplant Outcomes
Kelly E. Rea1, Kara B. West2,3, Anna Dorste4, Elizabeth Christofferson5,6, Debra Lefkowitz2,3, Emily Mudd7, Lauren Schneider8, Courtney Smith9,10, Kelli N. Triplett11,12, Kristine McKenna13.
1Department of Psychology , University of Georgia , Athens , GA, United States; 2Children's Hospital of Philadelphia, Philadelphia, PA, United States; 3Perelman School of Medicine at the University of Pennsylvania , Philadelphia, PA, United States; 4Boston Children's Hospital , Boston , MA, United States; 5 University of Colorado School of Medicine, Aurora, CO, United States; 6Children's Hospital Colorado, Aurora, CO, United States; 7Center for Pediatric Behavioral Health , Cleveland Clinic Children's, Cleveland , OH, United States; 8Stanford University School of Medicine, Palo Alto, CA, United States; 9Norton Children's, Louisville, KY, United States; 10University of Louisville , Louisville, KY, United States; 11Children's Health, Children's Medical Center Dallas, Dallas, TX, United States; 12Department of Psychiatry , University of Texas Southwestern , Dallas, TX, United States; 13Seattle Children's Hospital , Seattle , WA, United States
Introduction: Equitable access to pediatric organ transplantation is critical, though risk factors negatively impacting pre- and post-transplant outcomes remain. No synthesis of the literature on social determinants of health (SDoH) within the pediatric organ transplant population has been conducted; thus, the current systematic review summarizes findings to date assessing SDoH in the evaluation, listing, and post-transplant periods.
Methods: This systematic review was conducted in accordance with PRISMA guidelines. Comprehensive search strategies were created for Web of Science, Embase, PubMed, and Cumulative Index to Nursing and Allied Health Literature, including controlled vocabulary terms from each database combined logically with keywords using Boolean Logic. Terms were extracted per the following concepts: pediatrics, organ transplantation, disparities, and identity. Database results were extracted and deduplicated in EndNote following validated deduplication methods.
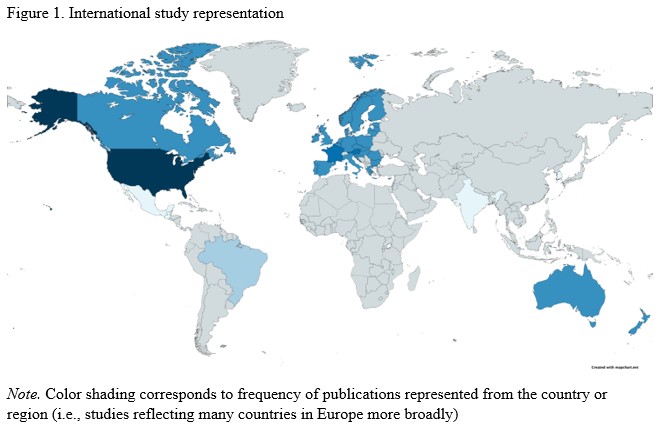
Results: Ninety-three studies were included based on pre-established criteria and were reviewed for main findings and study quality. Most studies were in kidney transplant (n=61, 70%), with liver (n=16, 17%), heart (n=11, 12%), and multi-organ (n=1, 1%) also represented. Half were published within the last five years (n=47, 51%), with the majority in the last decade (n=80, 86%). Most studies used data solely from the United States (n=55, 59%) or from a combination of US and other countries and territories (e.g., Canada, Mexico, Puerto Rico, Costa Rica; n=7, 8%), and the remaining n=31 (33%) used data solely from countries outside of the United States. See Figure 1 for international study representation.
Findings consistently demonstrated disparities in key transplant outcomes based on racial or ethnic identity, including timing and likelihood of transplant, and rates of rejection, graft failure, and mortality. Though less frequently assessed, variation in outcomes based on geography were also noted, while findings related to insurance or socioeconomic status were inconsistent.
Conclusion: This review underscores the persistence of SDoH and disparity in equitable transplant outcomes and discusses the importance of individual and systems-level change to reduce such disparities. Recommend transplant teams engage in efforts to improve research via development of comprehensive models rather than exploration of SDoH in isolation and through multi-center collaboration. Additionally, recommend transplant teams take steps to reduce bias in clinical care by recognizing aspects of clinical workflow that contribute to systemic racism and health disparities (e.g., use of patient/family advisory councils, education related to implicit and explicit bias, etc.).