A case of native kidney post-transplant lymphoproliferative disorder and BK nephropathy after orthotopic heart transplantation
Yitong Liu1, Kevin Barton1, Vikas Dharnidharka1, Raja Dandamudi1.
1Department of Pediatrics, Division of Nephrology, Hypertension & Pheresis, Washington University School of Medicine in St. Louis, St. Louis, MO, United States
Post-transplant lymphoproliferative disorder (PTLD) is an important complication of solid organ transplantation. It is a malignancy commonly associated with EBV infection and resultant B cell transformation. Transplant recipient seronegativity to EBV, pediatric age, thoracic organ or intestinal transplant, and potent immunosuppression are recognized risk factors of PTLD. There are reports of PTLD development in the allograft kidney, as well as rare reports of PTLD in a native kidney after liver and kidney transplant but none after heart transplantation. BK virus nephropathy (BKVN) is an important cause of graft dysfunction and morbidity in kidney transplant. Native kidney BKVN, on the other hand, is a noted cause of chronic kidney disease and is diagnosed later and is a rare entity after thoracic transplantation. We present a case here of PTLD and BKVN in a native kidney after orthotopic heart transplantation.
Patient is a 4 year old female with complex congenital cardiac anomalies of DORV, hypoplastic LV status post heart transplant 2 years prior to presentation. Post-transplant course was complicated by AMR 10 months after transplant, for which she received TPE, corticosteroids, rituximab, and bortezumab therapy for non-HLA, AT1R-positive, AMR with resolution on follow-up biopsy as well as primary EBV infection.
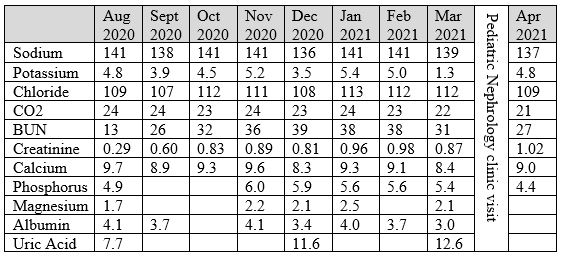
She was noted to have rising creatinine from a baseline of 0.3-0.4 to 0.9 mg/dL over several months with elevated uric acid between 7.7 and 12.6 mg/dL. Renal ultrasound was notable for bilaterally enlarged and echogenic kidneys. Based on these findings, her renal symptoms were attributed to chronic calcineurin inhibitor toxicity. Her immunosuppression regimen at that time included tacrolimus, everolimus, and prednisolone (previously tacrolimus, MMF, and prednisolone).
She was subsequenytly admitted due to concern for rejection with abdominal distension and elevated BNP, and was started on a course of thymoglobulin and TPE due to history of severe AMR. She underwent a kidney biopsy due to acutely worsened creatinine after admission, which was consistent with BKVN and PTLD. Accordingly, immunosuppression was simplified to everolimus only and she was started on IVIg infusions and chemotherapy (rituximab, prednisone, and cyclophosphamide). She required renal replacement therapy due to fluid overload with chemotherapy, but was able to transition to chronic diuretic therapy. She subsequently had exacerbation of heart failure symptoms, and unfortunately suffered a code event during cardiac catheterization with multisystem organ failure so was redirected to comfort care in accordance with the family’s wishes.
This case reiterates the importance the consideration of renal PTLD and BKVN even in non-kidney transplant patients. While these entities are rare in non-kidney transplant recipients, they confer high morbidity and poor outcomes.
[1] Araya CE, Mehta MB, Gonzalez-Peralta RP, Hunger SP, Dharnidharka VR. Native kidney post-transplant lymphoproliferative disorder in a non-renal transplant patient. Pediatric Transplantation. 2009; 13(4): 495-498.
[2] Dharnidharka VR. Epidemiology of PTLD after SOT. Post-Transplant Lymphoproliferative Disorders. 2021: 111-128.
[3] Smith JM, Dharnidharka, VR. Prevention and treatment of infectious complications in pediatric renal transplant recipients. Pediatric Kidney Disease. 2016:1875-1889.
[4] Maxwell H, Webb NJA. Chronic renal transplant dysfunction. Pediatric Kidney Disease. 2016: 1833-1873.