Transition from paediatric to adult services: a new model for renal transplant recipients following the COVID-19 Pandemic
Helen Jones1, Nicholas Ware1, Louise Kipping1, Wilson Wong2, Paul N. Harden3, Hannah Kilbride4, Ed Kingdon5, Joyce Popoola6, Fiona Harris7, Mark Andrews8, Arran Wheatley1, Grainne Walsh1.
1Department of Paediatric Nephrology, Evelina London Children's Hospital, London, United Kingdom; 2Department of Nephrology, Guy's Hospital, London, United Kingdom; 3Department of Nephrology, Churchill Hospital, Oxford, United Kingdom; 4Department of Nephrology, Kent and Canterbury Hospital, Canterbury, United Kingdom; 5Department of Nephrology, Royal County Sussex Hospital, Brighton, United Kingdom; 6Department of Nephrology, St George's Hospital, London, United Kingdom; 7Department of Nephrology, St Helier Hospital, Carshalton, United Kingdom; 8Department of Nephrology, Norfolk and Norwich University Hospital, Norwich, United Kingdom
Introduction: Our service development arose from the COVID-19 pandemic, a time when our young transplant recipients were classified as extremely vulnerable and face to face (F2F) clinic visits were limited. Prior to the pandemic we held multidisciplinary joint F2F clinics with both paediatric and adult colleagues present in the majority of cases. These were paused during the pandemic and our model of transition revised to ensure patients still underwent a smooth transfer.
Here we describe the set-up which has existed since the onset of the COVID-19 pandemic.
Methods: We reviewed the transition pathway for paediatric renal transplant recipients transferred to adult services since March 2020.
Results: Between March 2020 and September 2022, 31 patients transferred to 7 adult transplant centres over a large geographical area. The model for their transfer appointment is summarised in the table below.
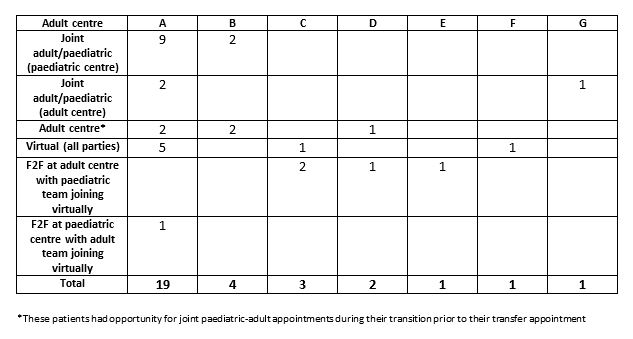
19/31 of the patients transferred to the adult services in the tertiary centre where they underwent paediatric nephrology follow up (centre A). The bi-monthly young adult clinic held jointly between paediatric and adult services within the adult renal clinic setting was paused between March 2020 and October 2021 when it then resumed. An adolescent clinic was held 3 times a year within the paediatric centre with adult nephrology colleagues from centre A. This was cancelled in March 2020 and re-started in November 2020, after which 9 patients transferred to adult services.
The other 12/31 patients transferred to 6 other transplant centres in a variety of F2F and virtual clinics.
5 patients had their transfer appointments in the adult transplant centre without a member of the paediatric team present. In all cases patients had had previously had the opportunity to meet jointly with the paediatric and adult transplant teams as part of the transition process.
In 11/31 transfer appointments a virtual clinic platform was used to facilitate the patients transfer to adult services, and in 7/11 of these cases all parties (the patient, the parent(s) and professionals) joined virtually.
Conclusion: The COVID-19 pandemic made transferring paediatric transplant recipients to adult transplant services very challenging due to a reduction in face to face clinics, however we were able to utilise the novel virtual clinic platforms.
These enabled flexibility with their appointments, which were time and cost saving to both patients, staff and their departments, with patients being able to reduce the time they missed from school or work. It also gave more opportunity to have virtual clinics with patients who don’t attend the paediatric clinic frequently to see them for transition planning as well as involving the adult service.
As a result our service has become much more individualised, particularly in the year before and after transfer when virtual appointments facilitate extended shared care.