Long-term neurodevelopmental outcomes following liver transplantation for metabolic disease
Catherine Patterson1,2,3, Anna Gold2,4, Stephanie So1,2,3, Eva Mamak4, Michaela Dworsky-Fried2,5, Leila Kahnami4,6, Alaine Rogers1,2,3, Andreas Schulze7,8, Yaron Avitzur2,9.
1Department of Rehabilitation Services, The Hospital for Sick Children, Toronto, ON, Canada; 2Transplant and Regenerative Medicine Centre, Hospital for SickChildren, Toronto, ON, Canada; 3University of Toronto, Toronto, ON, Canada; 4Department of Psychology, The Hospital for Sick Children, Toronto, ON, Canada; 5Department of Psychology, University of Ottawa, Ottawa, ON, Canada; 6Department of Psychology, York University, Toronto, ON, Canada; 7Division of Clinical and Metabolic Genetics, The Hospital for Sick Children, Toronto, ON, Canada; 8Departments of Pediatrics and Biochemistry, University of Toronto, Toronto, ON, Canada; 9Division of Gastroenterology, Hepatology and Nutrition, The Hospital for Sick Children, Toronto, ON, Canada
Introduction: Inborn errors of metabolism (IEM) including urea cycle disorders (UCD) and organic acidemias (OA) often result in metabolic decompensations and subsequent neurological injury and developmental delay. Liver transplant (LT) can improve metabolic control and potentially mitigate longer term developmental sequalae. This study describes the neurodevelopmental outcomes within a cohort of children with IEM at 1-year and 3-years’ post-LT utilizing standardized motor and cognitive assessments.
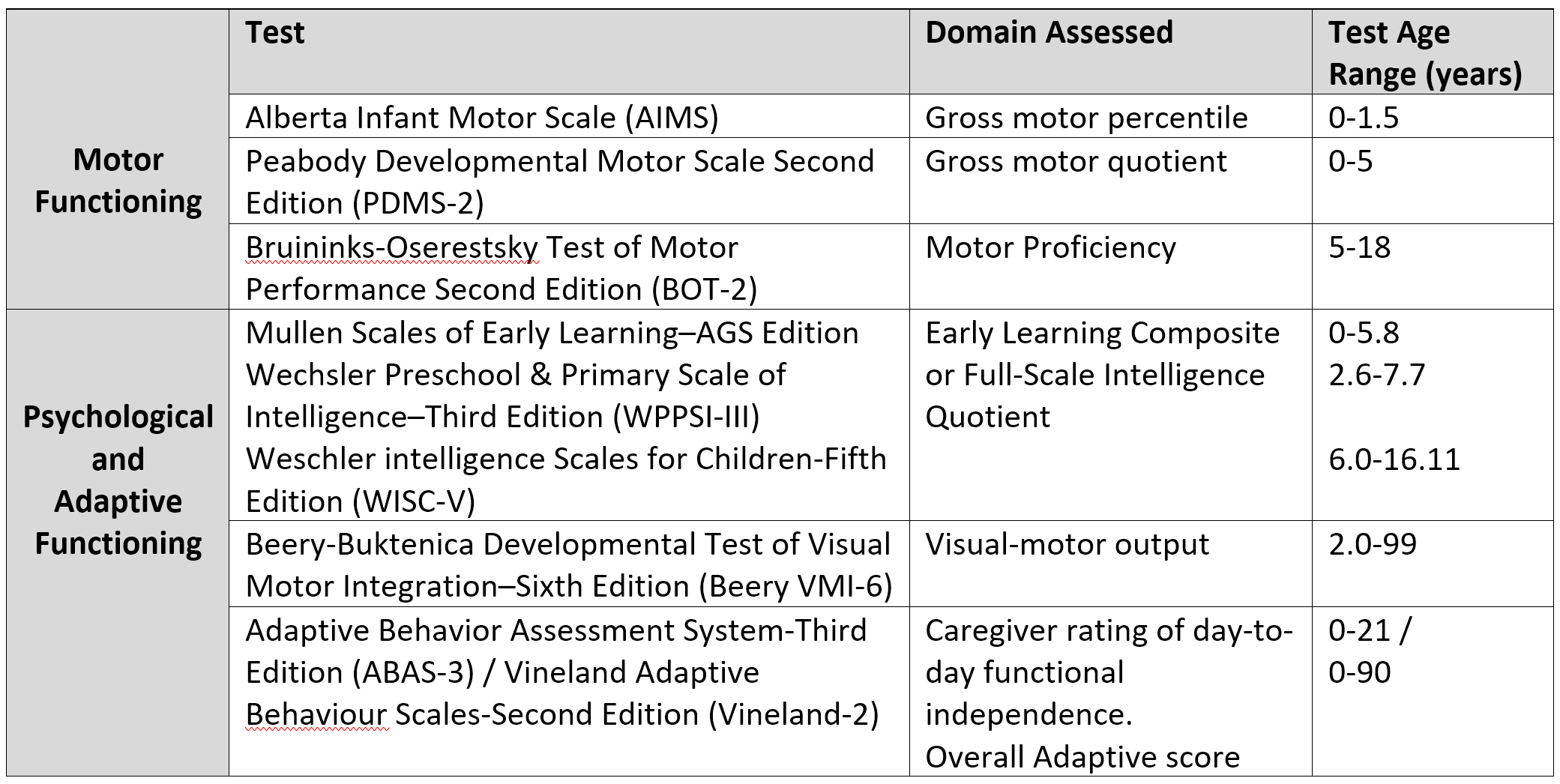
Methods: Retrospective chart review of children with an IEM diagnosis who underwent LT between January 2014-December 2021. Children without at least one motor or cognitive assessment were excluded. Cognitive assessments were initiated at 2.5 years of age. See Table 1 for assessment measures utilized. For analysis, children were grouped according to the following assessment outcomes: within age expectations (within 1 standard deviation (SD) of mean), at risk (1-2SD below mean) or delayed (>2SD below mean) compared to population norms.
Results: Twenty-four children (63% male) underwent LT with a median age at transplant of 1.4 (IQR 0.64, 4.36) years. Fifteen (63%) had a UCD diagnosis. Fourteen (58%) received a living donor transplant. Overall, 3-year survival rate was 100%. Fifteen (63%) required dialysis for hyperammonemia and 10 (42%) had documented seizures pre-LT.
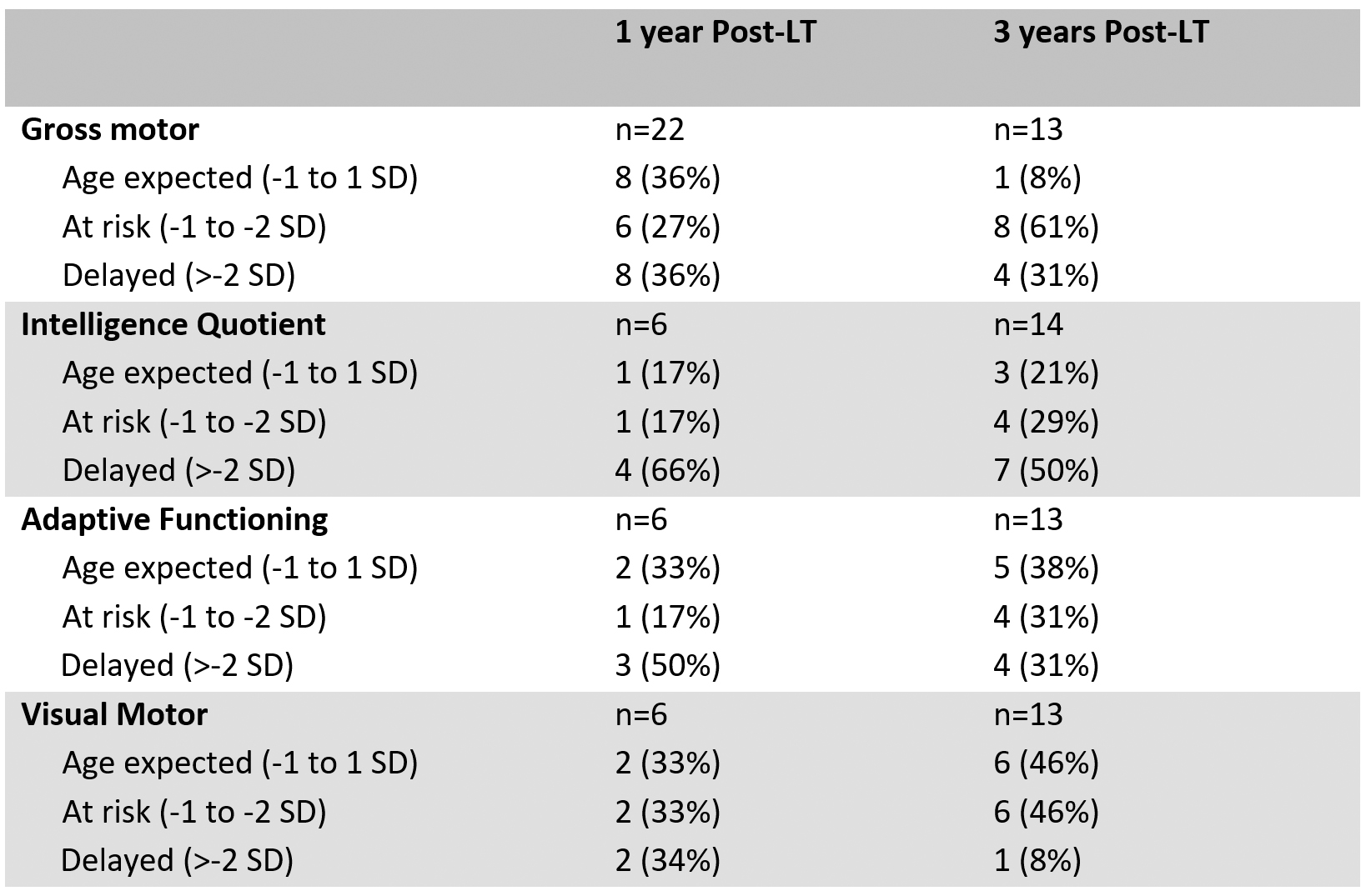
1-Year Post LT: Twenty-two children completed motor assessments, and 6 completed cognitive assessments. Overall, 14/22 (64%) had motor scores >1SD below mean and 5/6 (83%) had cognitive scores >1SD below mean (Table 2). 4/6 (67%) children were diagnosed with a Global Developmental Delay (GDD) / Intellectual Disability (ID) and 1/6 (17%) with Attention Deficit Hyperactivity Disorder (ADHD). At risk/delayed motor scores were associated with dialysis pre-LT (p=0.026); at risk/delayed visual motor scores were associated with admission for hyperammonemia pre-LT (p=0.067).
3-Years Post-LT: Thirteen children completed motor assessments and 14 completed cognitive assessments. 12/13 (92%) had motor scores >1SD below mean and 11/14 (78%) had cognitive measures >1SD below mean. 6/14 (43%) were diagnosed with GDD/ID, 1/14 (7%) with Learning Disability, 3/14 (21%) with ADHD, and 1/14 (7%) with Autism Spectrum Disorder. Overall prevalence of motor and cognitive delay along with psychological diagnosis is higher than population norms, and those reported for children post-LT with a non-IEM diagnosis. Lower intelligence scores were associated with a UCD diagnosis (p=0.024).
Conclusions: Higher prevalence of developmental impairment post-LT for IEM may reflect pre-LT related neurological pathology. However, in our study, the proportion of children falling within age expectation on cognitive measures increased at 3 years post-LT. Our results support the need for earlier screening and therapeutic interventions which may optimize the long-term outcome of these children.
[1] Patterson C, So S, Rogers A, Ng VL. Motor outcomes in young children pre-and one-year post-liver transplant. Pediatr Transplant. 2022;26(3):e14200. doi:10.1111/petr.14200
[2] Sorensen LG, Neighbors K, Martz K, et al. Longitudinal study of cognitive and academic outcomes after pediatric liver transplantation. J Pediatr. 2014;165(1):65-72.e2. doi:10.1016/j.jpeds.2014.03.032
[3] Sorensen LG, Neighbors K, Zhang S, et al. Neuropsychological functioning and health-related quality of life: pediatric acute liver failure study group results. J Pediatr Gastroenterol Nutr. 2015;60(1):75-83. doi:10.1097