
Are hemodynamic targets related to renal-injury biomarker excretion during pediatric kidney transplantation?
Marieke Voet1, Dirk van Lier2, Joris Lemson2, Alex Zarbock4, Marlies E.A. Cornelissen3, Peter Pickkers2.
1Anesthesiology, Pain and Palliative Care, Radboud university medical center, Nijmegen, Netherlands; 2Intensive Care Medicine, Radboud university medical center, Nijmegen, Netherlands; 3Pediatric Nephrology, Radboud university medical center, Nijmegen, Netherlands; 4Anesthesiology, Critical Care and Pain Medicine, University Hospital, Münster, Germany
Introduction: The large donor-acceptor size-mismatch in kidney transplantation with young acceptor and adult donor, requires significant increases in the acceptors cardiac output and blood pressure to optimize donor-kidney perfusion. Therefore, perioperative supraphysiological hemodynamic targets are recommended in most protocols. Often, liberal administration of fluids and vasopressor therapy are needed to reach targets, risking fluid overload and limited graft perfusion(1). To evaluate the effects of this approach on post-ischaemic kidney injury, we analysed postoperative renal-injury biomarker profiles in relation to hemodynamic variables(2, 3).
Methods: Observational, single centre study. Patient characteristics, hemodynamic variables, norepinephrine infusion rates, fluids, urine output and renal clearance data were collected. By protocol, hemodynamic management was guided by target cardiac index(CI) >3.5 L/min/m2 and mean arterial pressure(MAP) >65 mmHg. Urine samples were taken from four hours postreperfusion until three days postoperative at 8-12-hour intervals. Biomarkers KIM-1, NGAL, LFABP, IGFBP-7 and TIMP-2 were analysed with commercially available ELISA kits. Data analysis included correlation analyses of total splint urine biomarker excretion with perioperative CI, MAP, central venous pressure (CVP) and norepinephrine infusion rates.
Results: Fifteen patients were included with mean [IQR] age 6 [5-8] years, weight 21[16‑25] kg and donor/acceptor BSA-mismatch of 2.4 [2.1-3.0]. All patients had diuresis within one hour after kidney reperfusion and good renal function at discharge.
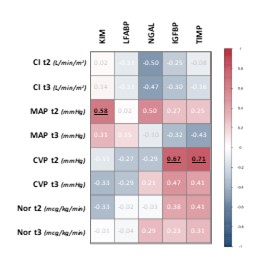
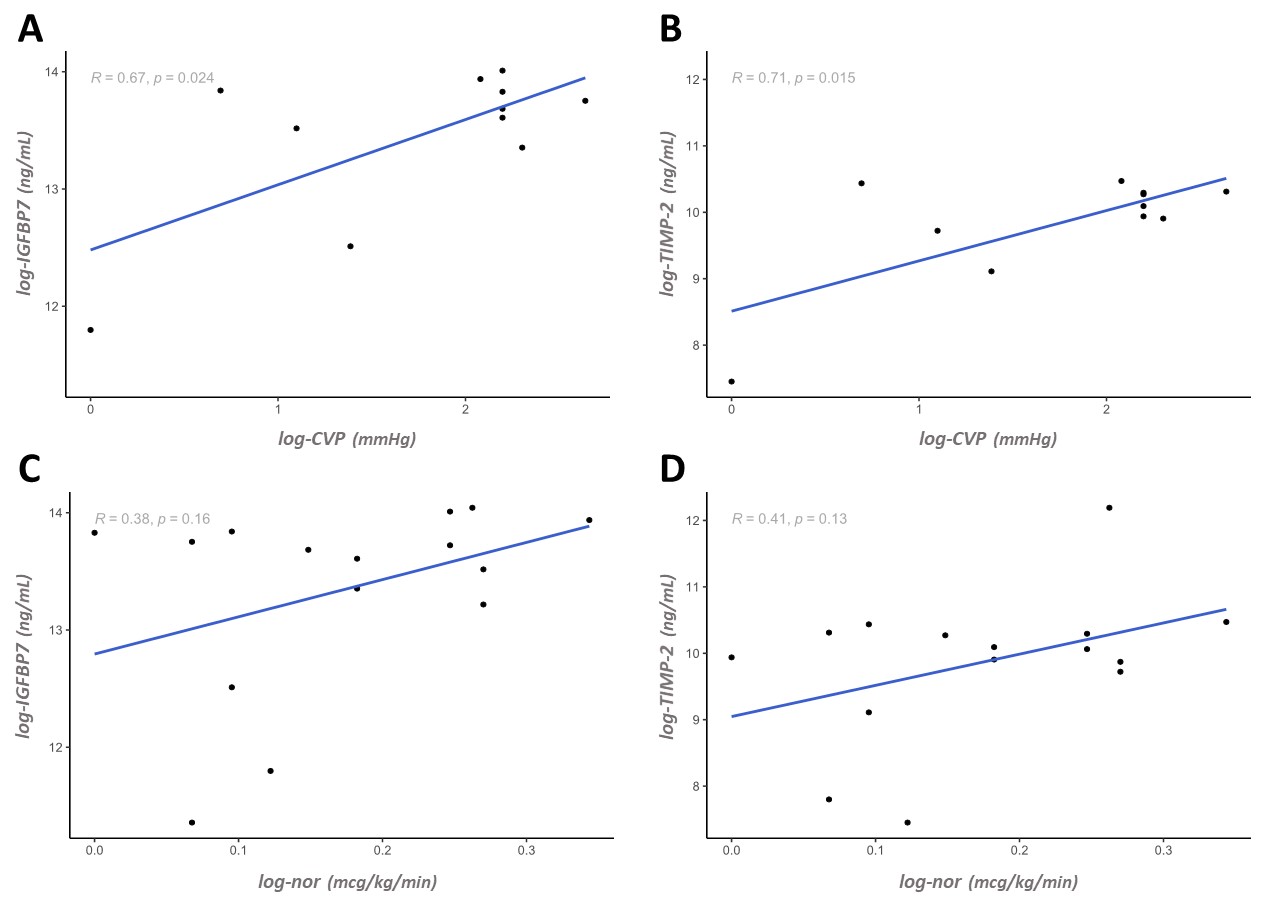
No relevant trends in correlations of cardiac output or MAP with renal-injury biomarker excretion were found for any of the investigated biomarkers at any of the postoperative timepoints (Figure 1). Correlation analyses showed significant associations of CVP with IGFBP-7 (r0.67, p=0.02) as well as TIMP-2 (r0.71, p=0.02) (Figure 2, panel A/B). Norepinephrine infusion rates showed a positive trend, but associations were not statistically significant; r0.38, p=0.16 for IGFBP-7 and r0.41, p=0.13 for TIMP-2 (Figure 2, panel C/D). Both CVP and norepinephrine showed no associations with KIM-1, NGAL or LFABP (Figure 1).
Conclusion: CVP was positively correlated, and norepinephrine infusion rates showed a positive trend, with excretion of renal-injury biomarkers IGFBP-7 and TIMP-2. Cardiac output and MAP showed no correlation with any of the biomarkers. These results suggest that careful titration of fluids and vasopressors is essential, while no benefit was observed in aiming for a supraphysiological cardiac output in kidney transplantation with large donor‑acceptor size mismatch.
Sectie Kinderanesthesiologie, Nederlands Vereniging voor Anesthesiologie.
[1] 1. Voet M, Cornelissen EAM, van der Jagt MFP, Lemson J, Malagon I. Perioperative anesthesia care for the pediatric patient undergoing a kidney transplantation: An educational review. Paediatric anaesthesia. 2021;31(11):1150-60.
[2] 2. Bennett MR, Nehus E, Haffner C, Ma Q, Devarajan P. Pediatric reference ranges for acute kidney injury biomarkers. Pediatr Nephrol. 2015;30(4):677-85.
[3] 3. Sandokji I, Greenberg JH. Novel biomarkers of acute kidney injury in children: an update on recent findings. Curr Opin Pediatr. 2020;32(3):354-9.