Predictors for pathological bone fractures in children undergoing liver transplantation
Damiano Astolfi1, Nathalie Rock1, Valérie A. McLin1, Dimitri Ceroni1, Barbara E. Wildhaber1.
1Department of Pediatrics, Gynecology, and Obstetrics, University Hospitals of Geneva, Geneva, Switzerland
Introduction: Bone disorders is a common condition observed in children undergoing liver transplantation (LT). Hepatic osteodystrophy is a generic term encompassing all the bone anomalies associated with chronic liver disease, physical inactivity, sarcopenia, metabolic disorders, and kidney insufficiency. It may lead to decreased bone mineral density, rickets, growth failure, and to pathological fractures (PF). The aim of this study was to identify predictive factors for PF to improve their prevention in children before and after LT.
Methods: Children aged 0 to 16 years undergoing LT at the Swiss Pediatric Liver Center from January 2005 to December 2020 were included. Patients with multiple LT and who died before 1 year post-LT were excluded. Data on patient demographics, injury mechanisms and trauma circumstances, and biological workups were extracted. Variables were assed at 3 time points: T1 at the moment of listing for LT; T2 at the moment of LT, and T3 at 1-year post-LT. PF were defined as any fractures occurring without adequate trauma before and/or after LT. Nutritional support was defined as partial or total administration of caloric needs by nasogastric tube or parenteral nutrition. Ethical approval was obtained from the local ethics committee.
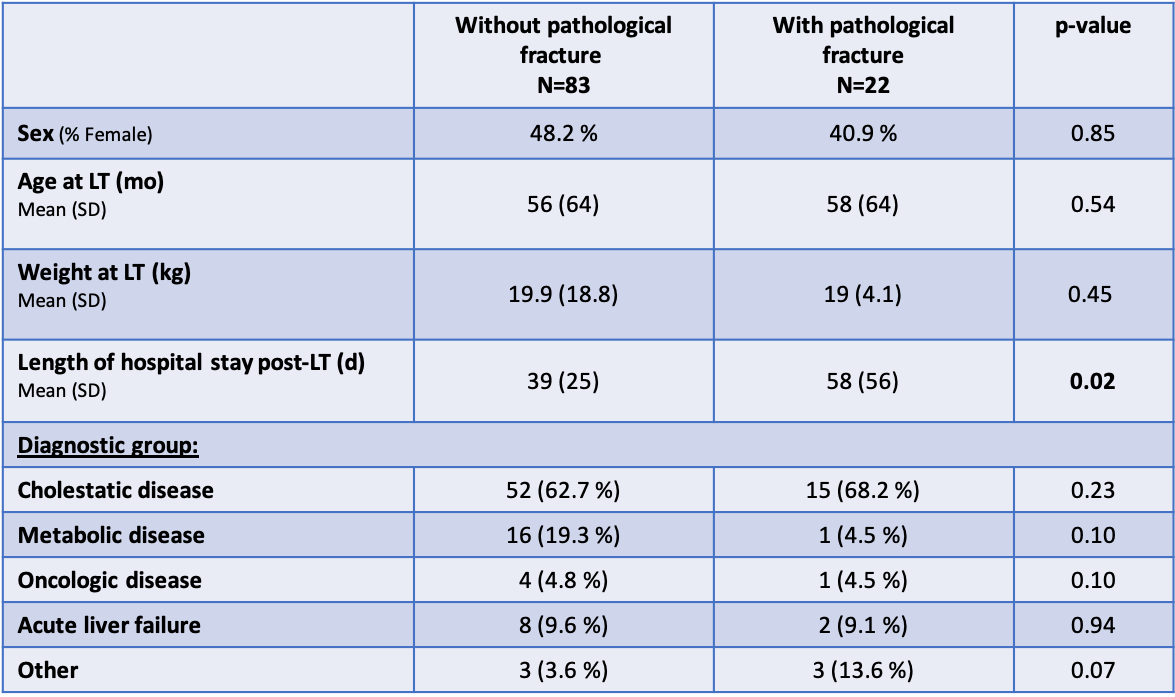
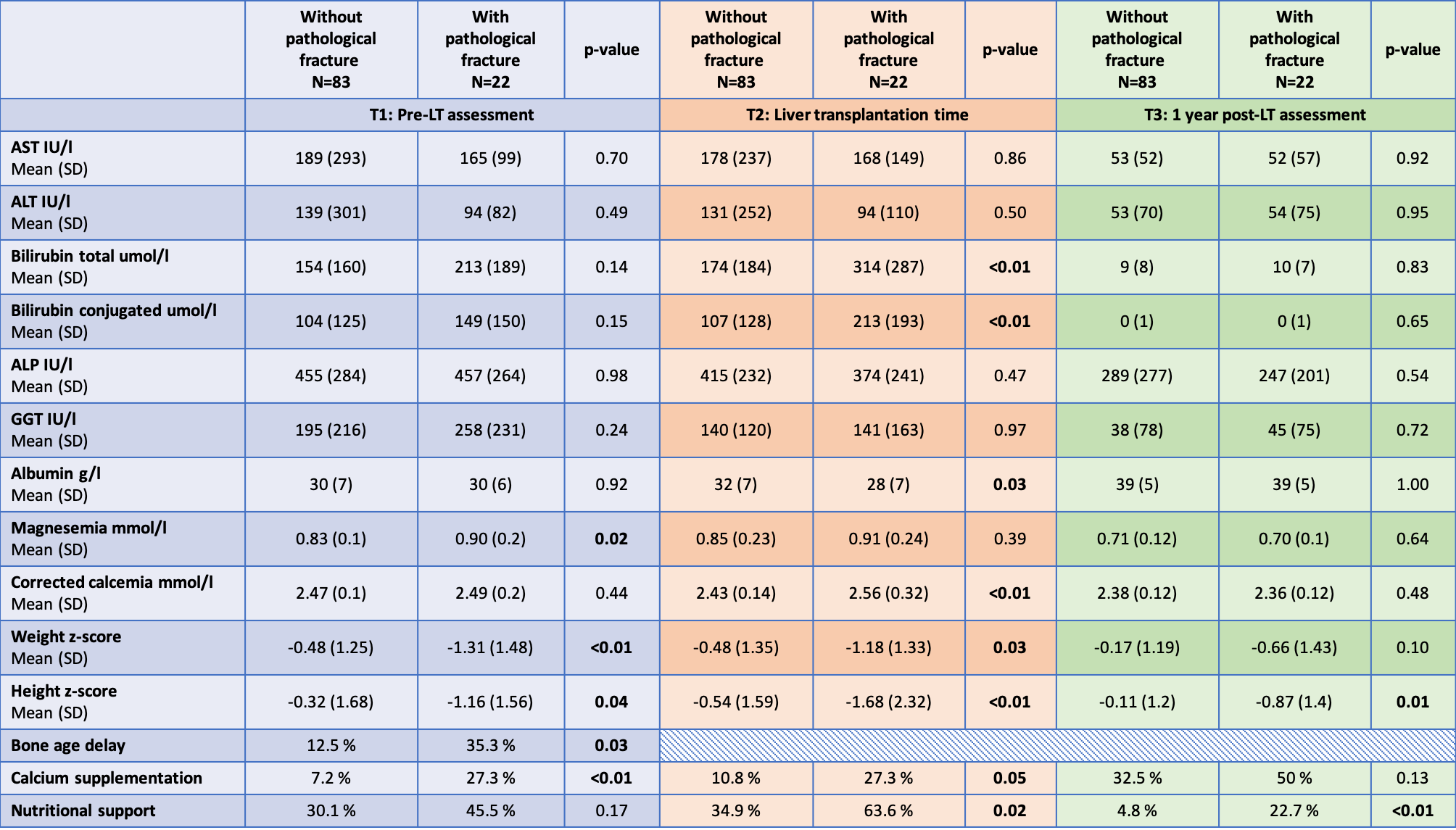
Results: A total of 105 children were included in this study. Twenty-two patients (21%) experienced 65 PF, which affected long bones in 43 cases (66%), and flat bones in 22 cases (34%). Fourteen children presented PF just before or during the hospital stay for LT, 7 only after LT (up to 7.5 years post LT), 1 before and after LT; 7 of them had several events of fractures. Table 1 summarizes patient demographics. Variables significantly associated with the occurrence of PF were at T1: higher serum Mg, lower weight and height z-score, bone age delay and being under Ca supplementation. At T2, the following variables were suggestive to be significantly associated with PF: higher total and conjugated bilirubin, higher serum Ca, lower serum albumin, lower weight and height z-score, bone age delay and being under Ca supplementation and nutritional support. At T3 significant differences had weaned. Detailed findings are summarized in Table 2. Upon comparative analysis of patients experiencing PF with cholestasis versus those without cholestasis, cholestatic patients showed a trend to be younger at T1 (p<0.01) and have a trend for lower weight z-score at T1 (p=0.06).
Conclusion: One of five children needing LT will experience a PF during follow-up either before or after LT. Patients with a low z-score for weight and height, and a significant delay in bone age are at increased risk for PF. Nutritional support and Ca supplementation seemingly being associated with more PF indicates that even nutritional intervention before LT cannot counteract completely the effect of chronic hepatic osteodystrophy due to liver disease and chronic cholestasis causing malabsorption.