Effects of acuity circle liver allocation policy on pediatric whole liver transplants in high versus low volume transplant centers
Jacqueline Kim1,2, Tanveen Ishaque2, Jeffrey Stern1, Dorry Segev2, Adam Griesemer1, Allan Massie2.
1Transplant Institute, NYU Langone Health, New York, NY, United States; 2Center for Surgical & Transplant Applied Research, NYU Langone Health, New York, NY, United States
Background: Pediatric transplant candidates have historically been disadvantaged on the transplant waitlist, with nearly half of pediatric deceased donor organs allocated to adult recipients (Hsu, Gastroenterology, 2017), and allocation pediatric end-stage liver disease (PELD) scores that underestimate children’s expected 3-month mortality compared to that of adult patients (Chang, JAMA Pediatrics, 2018). Disparities in organ distribution prompted revision of the liver allocation policy in 2020 from donation services areas (DSA) to a series of distance-based concentric circles called acuity circles (AC) before being offered nationally (US GAO, 2022), which was designed to minimize geographic inequity in liver transplant. Prior to implementation of the new liver allocation policy, analysis using the Liver Simulated Allocation Model projected that AC allocation would decrease disparities for pediatric liver transplant candidates and recipients by increasing transplants and decreasing waitlist mortality (Mogul, Transplantation, 2020). In this study, we evaluate differences in pediatric whole liver transplants performed before and after the implementation of acuity circle liver allocation policy.
Study Design: We evaluated patient characteristics, adjusted MELD/PELD at time of transplant, calculated donor age at time of transplant among pediatric whole liver transplant recipients in low versus high-volume pediatric liver transplant centers performed before and after implementation of AC-based liver allocation policy using the Scientific Registry of Transplant Recipients.
Results: Before and after the implementation of ACs, differences in pediatric liver transplants by age group (<2 years, 2-5 years old, 5-12 years old, and 12-18 years old) remained significantly different between low and high-volume pediatric transplant centers. Under DSA allocation policy, the median MELD/PELD at transplant was 37.0 (IQR 30.0-41.0) in low-volume centers and 40.0 (IQR 30.0-41.0) in high-volume centers. After the implementation of acuity circles, median MELD/PELD at transplant decreased to 35.0 (IQR 21.0-41.0) in low-volume centers and 35.0 (IQR 25.0-41.0) in high-volume centers. Finally, donor age at time of transplant increased from 8.0 (IQR 2.00-18.0) to 13.5 (IQR 4.5-21.0) at low-volume centers, and from 3.0 (IQR 1.0-14.0) to 4.0 (IQR 1.0-14.0) at high-volume centers before and after the implementation of ACs.
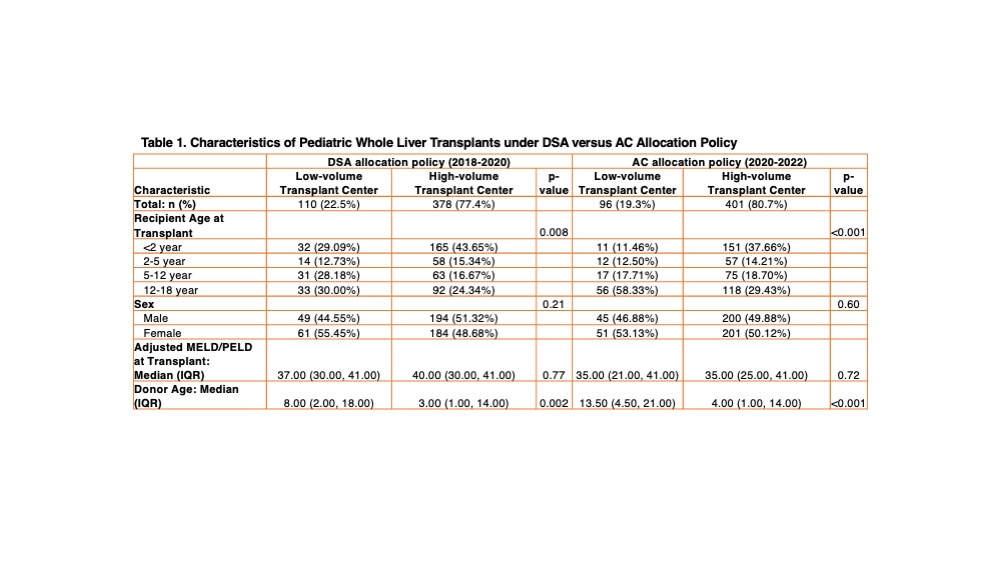
Conclusion: The change from DSAs to ACs in allocation policy and the shift from regional to national review boards have affected the characteristics of organ recipients, adjusted MELD/PELD at time of transplant, and donor age at time of transplant differentially between whole liver transplant recipients at low- and high-volume pediatric liver transplant centers.