Long-term outcomes following LDL apheresis in treatment-refractory recurrent focal segmental glomerulosclerosis
JoAnn Morey1, Michael Somers1,2.
1Division of Nephrology, Boston Children's Hospital, Boston, MA, United States; 2Department of Pediatrics, Harvard Medical School, Boston, MA, United States
Introduction: Recurrent focal segmental glomerulosclerosis (FSGS) complicates kidney transplantation in up to half of children with FSGS who progress to kidney failure and in up to 90% of those with prior transplant FSGS recurrence. FSGS recurrence increases post-transplant morbidity and has adverse effects on graft survival. Although plasmapheresis and immunosuppression intensification are mainstays of treatment for recurrent FSGS, a significant proportion of those with recurrent disease are refractory to these therapies. LDL apheresis (LDL-a) has been proposed as an efficacious therapy in this setting, though there is limited data as to both its utility and longer-term outcomes.
Methods: We present three cases of recurrent FSGS after deceased donor pediatric kidney transplants. Two children had a prior history of post-transplant recurrence with graft loss despite plasmapheresis and immunosuppression intensification. With their current transplants, all demonstrated early recurrence with resistance to plasmapheresis therapy and augmentation of immunosuppression, including pulse steroids, cyclophosphamide, and B cell depletion. These children then started a 12-treatment trial of LDL-a over 9 weeks (2 sessions/week x 3 weeks; weekly x 6 weeks) in the setting of ongoing nephrosis and marked graft dysfunction. Baseline immunosuppression was maintained during LDL-a. Clinical parameters assessing treatment response were assessed over the LDL-a course and subsequent follow-up.
Results: All three children manifested resolved edema and partial remission of FSGS with significant improvement in graft function during the initial 12 treatments, leading to ongoing weekly treatments with maintained or improved clinical parameters of remission. The first child maintained a partial remission through 84 LDL-a treatments over 31 months but died from an unrelated medical condition. In the next two children, after improvement with LDL-a, B cell depletion that had previously been ineffective was repeated. Both children entered complete remission and were tapered off LDL-a within 6 further treatments and have remained fully in remission now for 25 and 39 months.
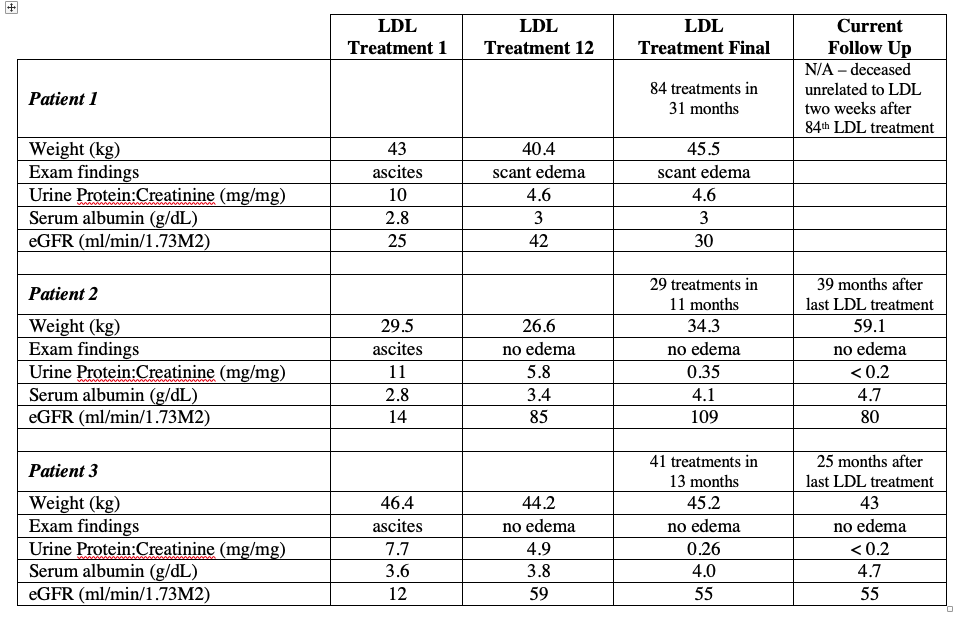
Conclusion: We conclude that: 1) LDL-a may be efficacious rescue therapy in treatment-refractory recurrent FSGS; 2) Remission achieved with LDL-a can be long-lived and complete even after LDL-a cessation; 3) Volume balance and graft function may improve significantly even with partial remission; 4) Prior ineffective therapies such as B cell depletion may exhibit better effect post-LDL-a.