Pediatric kidney transplant outcomes in recipients less than 10 kg in the United States
Stella Kilduff1,2, Nicole Hayde1,2.
1Pediatric Nephrology, The Children's Hospital at Montefiore, Bronx, NY, United States; 2Clinical Research , Albert Einstein College of Medicine, Bronx, NY, United States
Introduction: Pediatric kidney transplant (KT) was initially associated with poor outcomes, especially in smaller recipients due to increased risk of surgical and infectious complications [1, 2]. In more recent years, children as small as 7-8 kg may be considered for KT [3, 4]. The objective of our study was to assess the impact of weight at the time of transplant on renal transplant outcomes in pediatric KT recipients.
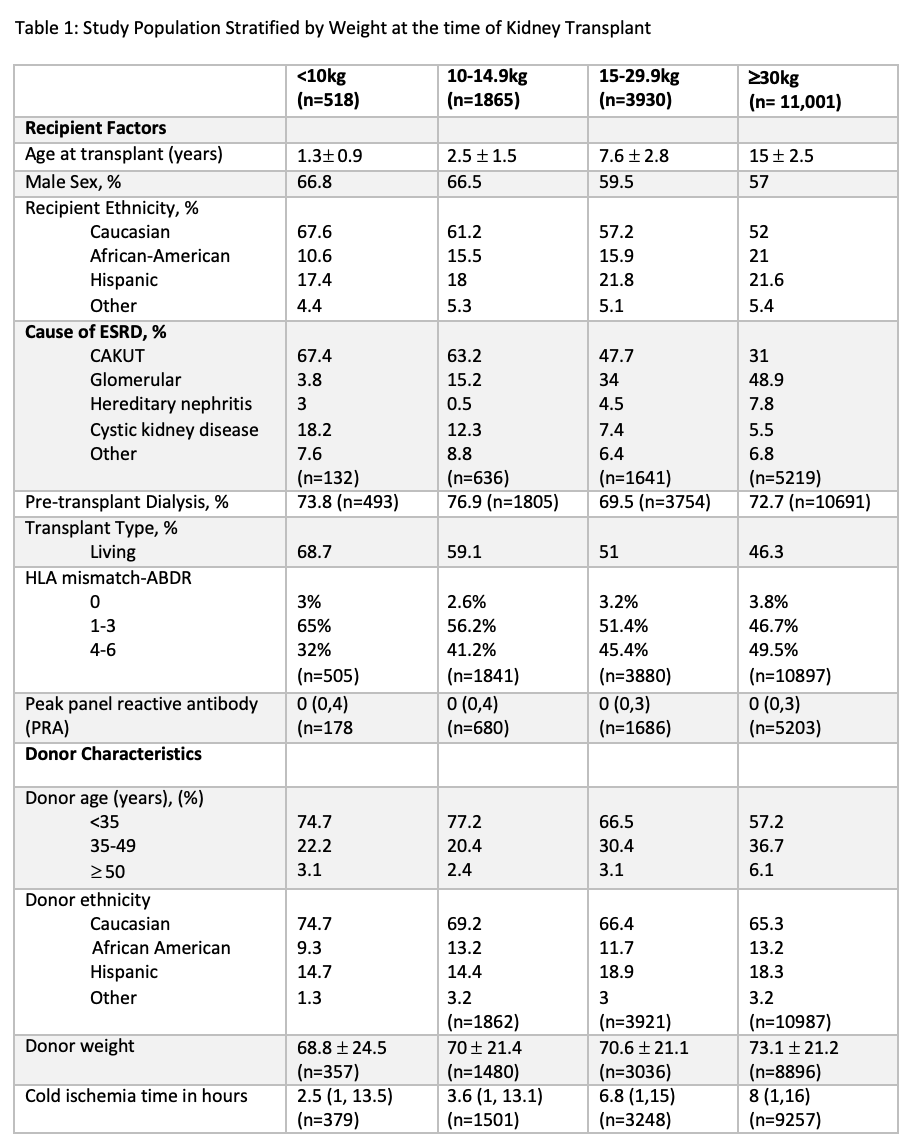
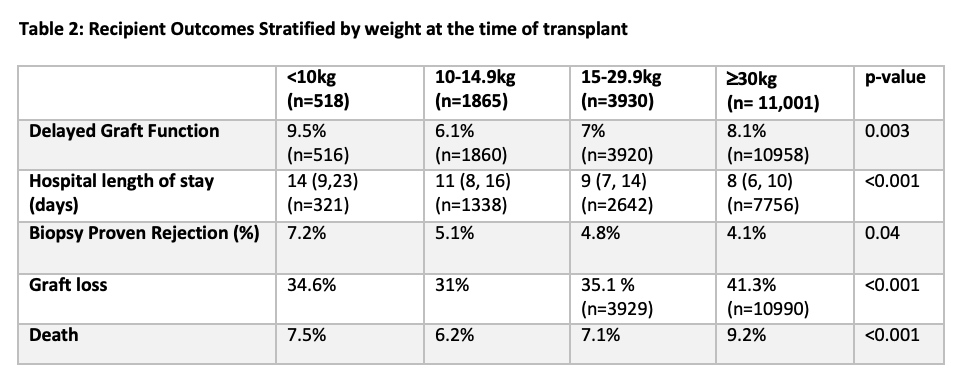
Methods: We conducted a retrospective study of all pediatric KT recipients in the United States performed between 1/1/99 and 12/31/14 using the United Network for Organ Sharing (UNOS) database. We sought to estimate differences in both patient and allograft survival in children (age <18 years) who were <10kg at the time of primary KT compared to those >10kg. Weight at the time of transplant was stratified into 4 groups: <10kg, 10-14.9kg, 15-29.9kg and >30kg. Clinical variables of interest were the type of transplant (living vs. deceased donor), delayed graft function (DGF) defined as the need for dialysis within the first week after kidney transplantation, the hospital length of stay (days), patient survival and allograft survival.
Results: A total of 16,834 pediatric KT recipients were eligible for study inclusion. When stratified according to weight, 518 (3%) recipients were <10kg (Figure 1). The mean age at the time of KT for the study population was 11.5 ± 5.4 years and the mean weight was 41.3 ± 21.8 kg. In the 518 recipients who were <10kg, their mean weight was 8.6 ± 1.2 kg and mean age was 1.3 ± 0.9 years. Transplant recipients <15 kg were more likely to receive a living donor. Figure 2 shows the clinical outcomes stratified by weight at the time of KT. The frequency of DGF was statistically significant between the 4 groups (however the frequencies were similar) and the median hospital length of stay (LOS) was significantly longer in children transplanted at <10kg [14 (9,23) days] and decreased as weight increased [>30kg group: 8(6,10) days; p<0.001]. The frequency of documented biopsy proven rejection was highest in the <10kg group but overall, the rates of rejection were similar between the 4 groups (range; 4.1-7.2%); p=0.04. There was a statistically significant difference in allograft loss across all 4 groups (p<0.001) with the highest proportion of allograft loss in the >30kg group (41.3% vs. 34.6% in the 10kg group). The time to allograft loss was significantly shorter with a median time of 4.2 (2.1, 7.5) years post-transplant in children transplanted >30 kg. The frequency of death was slightly higher in the >30 kg group (9.2% vs 7.5% in the <10kg group); p<0.001.
Conclusion: Children < 10kg at the time of KT had similar allograft outcomes to other weight groups. Future analyses will investigate how allograft survival changed over the study period (25 years) for recipients <10kg and determining whether weight at the time of transplant is an independent predictor of allograft survival.
NIH/National Center for Advancing Translational Science (NCATS) Einstein-Montefiore CTSA Grant Number UL1TR001073..
[1] Van Arendonk, K.J., et al., National trends over 25 years in pediatric kidney transplant outcomes. Pediatrics. 2014. 133(4): p. 594-601.
[2] Vitola, S.P., et al., Kidney transplantation in children weighing less than 15 kg: extraperitoneal surgical access-experience with 62 cases. Pediatr Transplant. 2013. 17(5): p. 445-53.
[3] Jalanko, H., I. Mattila, and C. Holmberg, Renal transplantation in infants. Pediatr Nephrol. 2016. 31(5): p. 725-35.
[4] Salvatierra, O., Jr., et al., Successful transplantation of adult-sized kidneys into infants requires maintenance of high aortic blood flow. Transplantation. 1998. 66(7): p. 819-23.