A pre-transplant risk assessment tool for outcome in pediatric kidney transplantation from a Dutch cohort of 1415 patients
Loes L Oomen1, Huib H de Jong2, Antonia AHM Bouts3, Mandy MG Keijzer-Veen5, Elisabeth EAM Cornelissen6, Liesbeth LL de Wall1, Wout WFJ Feitz1, Charlotte CMHHT Bootsma-Robroeks4,6.
1Urology, Radboudumc Amalia Children's Hospital, Nijmegen, Netherlands; 2Pediatric Nephrology, Erasmus MC-University Medical Centre, Rotterdam, Netherlands; 3Pediatric Nephrology, Amsterdam University Medical Center, Emma Children's Hospital, Amsterdam, Netherlands; 4Pediatric Nephrology, University Medical Center Groningen, Beatrix Children’s Hospital, Groningen, Netherlands; 5Pediatric Nephrology, University Medical Center Utrecht, Wilhelmina Children's Hospital, Utrecht, Netherlands; 6Pediatric Nephrology, Radboudumc Amalia Children's Hospital, Nijmegen, Netherlands
Introduction: Donor allocation is important in pediatric kidney transplantation. A prediction model for graft survival could assist to make a tradeoff between characteristics of available donors. The aim of this study is to develop a risk assessment tool for graft survival based on essential pre-transplantation characteristics.
Methods: Yearly registered data of a prospective national mandatory Dutch registry (NOTR) were used. A multivariable binary logistic model with discrete-time event history analysis was used to predict hazard of graft loss. Subsequently, a prediction score was calculated based on the B-coefficients. For internal validation a derivation (80%) and validation cohort (20%) were defined. Performance of the model was assessed with area under the curve (AUC) of the receiver operating characteristics curve (ROC), Hosmer-Lemeshow test and calibration plots.
Results: The model was based on 3179 observations after 1415 transplantations between 1966-2021. Graft loss occurred in 51% of the patients. Over time there was a significant increase in donor age, living and pre-emptive donations (p<0.05). In addition to these variables, recipient age, previous transplantations, number of HLA mismatches, duration of cold and warm ischemia, era of transplantation, time after transplantation and underlying disease were included in the model. The prediction formula based on this model was used to predict graft survival after transplantation (figure 1).
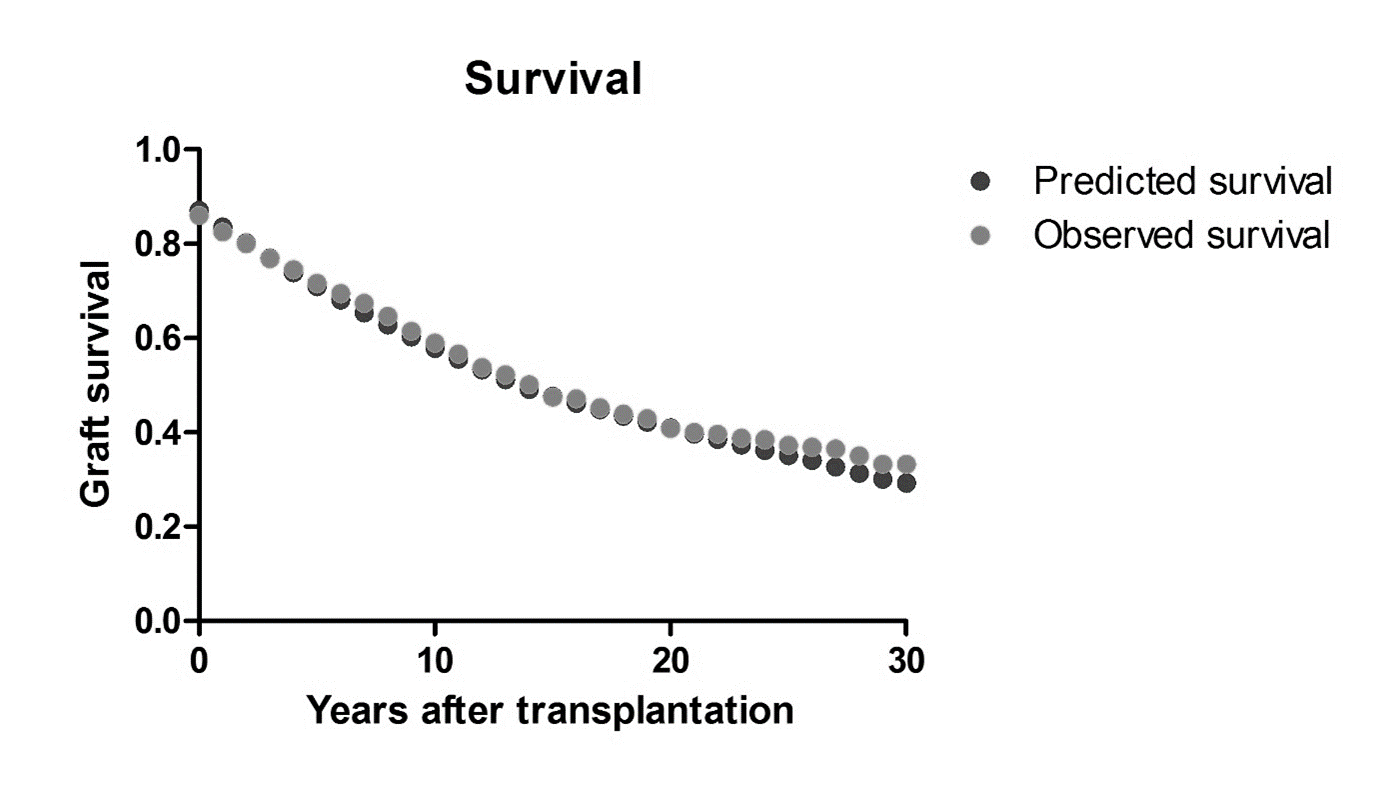
AUC in the derivation cohort was 0.84 and was 0.90 in the validation cohort. The predictive capacity of this model in the Netherlands was very good with AUC scores of 0.85, 0.80, 0.79 and 0.73 for 1, 5, 10 and 20 year graft survival respectively. Calibration plots showed excellent fit (figure 2).
Conclusion: This pediatric pre-transplant risk assessment tool was shown to be highly predictive for graft survival in the Netherlands. This model uses essential variables and could support decision making regarding donor selection and optimizing graft outcome.
Figure 1. Example of risk assessment of various hypothetical donors for a 12 years old recipient; first pre-emptive transplantation, nephrological origin of kidney failure HLA: human leucocyte antigen, DD: deceased donor, LD: living donor

Figure 2. Calibration plot. By the model predicted graft survival and observed graft survival in 1415 pediatric kidney transplantation.