Kidney Transplant Outcomes in the Pediatric and Young Adult Population with IgA Nephropathy
Rachel M. Engen1, Lyndsay A. Harshman 2, Jodi M. Smith3, James Perkins4, Sharon M. Bartosh1.
1Pediatrics, Nephrology, University of Wisconsin, Madison, Madison, WI, United States; 2Pediatrics, Nephrology, University of Iowa, Iowa City, IA, United States; 3Pediatrics, Nephrology, University of Washington, Seattle, WA, United States; 4Transplant Surgery, University of Washington, Seattle, WA, United States
Introduction: IgA nephropathy (IgAN) is characterized by a highly variable course with risk for post-transplant recurrence. Data are limited on the transplant outcomes among pediatric and young adults with IgAN.
Methods: Retrospective cohort study including patients aged 0 to 25 years from the Scientific Registry of Transplant Recipients between 10/1/1987 and 6/31/2021 who received a primary kidney transplant for IgA nephropathy or renal dysplasia. Primary outcomes included: 1) incidence of graft loss attributable to recurrence of IgAN and 2) the association between peri-transplant management and graft survival.
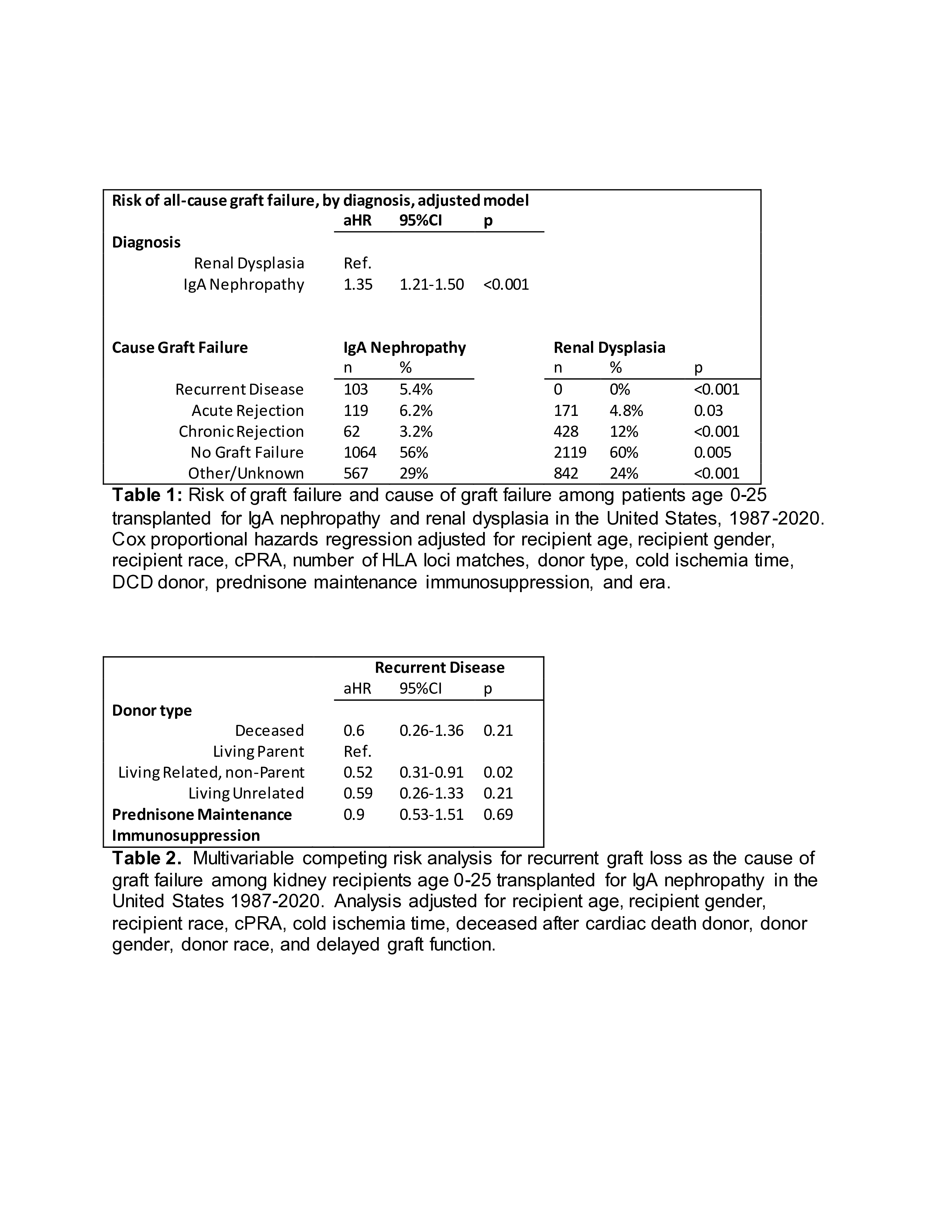
Results: 5475 transplant recipients were identified, including 1915 patients with IgAN and 3560 patients with renal dysplasia. In a multivariable Cox proportional hazards model, IgAN was associated with a higher risk of graft loss (aHR 1.35, 95%CI 1.21-1.50, p<0.001) compared to renal dysplasia (Table 1). Prednisone maintenance immunosuppression was not associated with superior graft survival (p=0.2). Graft loss due to recurrent disease was reported among 5.4% of patients with IgAN. In a multivariable competing risks analysis, IgAN patients receiving a parental living donor kidney were more likely to report graft loss from recurrent disease compared to those recipients of a living donor kidney from a nonparental relative (aHR 0.52 95%CI 0.31-0.91) p=0.02) (Table 2) . In analysis restricted to donor-recipient pairs matched at 3-6 HLA loci, incidence of graft loss due to recurrent disease was significantly higher among parental living donors (9.3%) compared to nonparental living related donors (5.1%), unrelated living donors (2.4%) or deceased donors (4.5%) (p=0.02). Overall graft survival remained higher among those with a 4-6 loci HLA matched kidney (aHR for graft failure 0.78 (95%CI 0.65-0.93) p=0.005) compared to those matched at 0-2 or 3 HLA loci, regardless of donor type.
Conclusion: In IgAN, utilization of a parental living donor is associated with a higher risk of graft loss due to recurrent disease. Despite this, overall graft survival remains higher with increased HLA matching. Individuals receiving a parental living donor allograft should have increased monitoring for recurrent disease, but maintenance prednisone immunosuppression does not improve graft survival.