Extended fibrosis in renal biopsy after kidney transplantation in recipients with methyl-malonic acidemia: just an illusion?
Samantha Innocenti1,2, Claire Tassin3, Anais Brassier4, Florence Lacaille5, Manuel Schiff4, Olivia Boyer1, Julien Hogan6, Jean Paul Duong Van Huyen3, Marion Rabant3, Laurène Dehoux1.
1Pediatric Nephrology Department, Hopital Necker Enfants Malades, Paris, France; 2Nephrology and Dialysis Department, Meyer Children's Hospital, Firenze, Italy; 3Department of Anatomopathology, Hopital Necker Enfants Malades, Paris, France; 4Metabolic Diseases Department, Hopital Necker Enfants Malades, Paris, France; 5Pediatric Hepatology and Gastro-enterology Department, Hopital Necker Enfants Malades, Paris, France; 6Pediatric Nephrology Department, Hopital Robert Debré, Paris, France
Introduction: A frequent complication of methyl malonic acidemia (MMA), a rare metabolic disease, is chronic kidney disease with about 14% of patients evolving to end stage kidney disease and needing a kidney (KT) or liver/kidney (LKT) transplantation. However their kidney transplant biopsies (KB) seemed to have more renal fibrosis lesions compared to KB of patients with other diseases. The aim of this study is to find if the evolution of MMA patients transplant kidney is different compared to other patients.
Methods: Retrospective case-control study comparing KB at 3 months and 12 months after transplantation between MMA patients and control group patients who received KT for congenital anomalies of kidney and urinary tracts. We included all the MMA patients with KT or LKT followed in Necker Hospital, Paris (France), from January 2001 to March 2022. Each patient was matched in KT year, donor and recipient age. All kidney biopsies slides were blinded reviewed by two renal pathologists. All data are expressed in mean with standard deviation and were compared using Z-score test or t-Student test (p< 0,05).
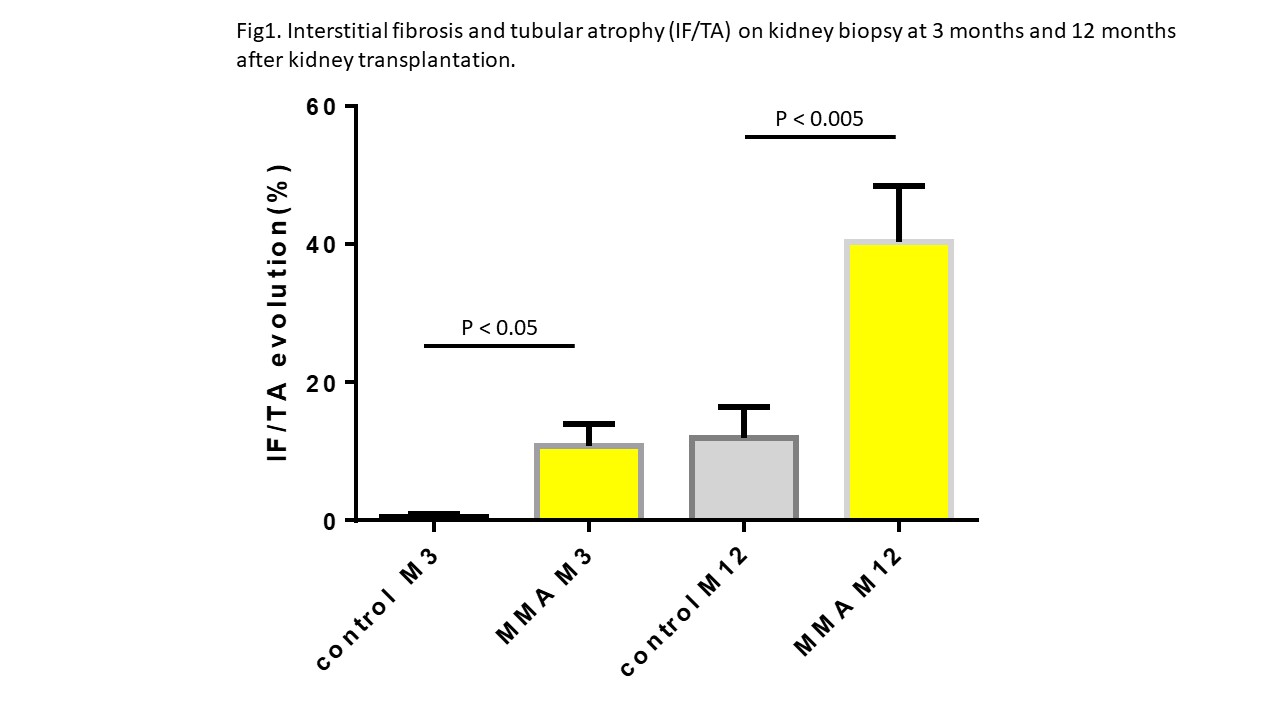
Results: We included 20 MMA patients (6 KT and 14 LKT) and 20 KT patients as control. KT or LKT mean age was 10 years (range 3-30 years). In MMA patients, a significant higher percentage of IF/TA were found compared control patients at 3 months (10,8%±12.7 vs 0.5% ±1.9, p=0,014) and 12 months (40.3%±31.5 vs 12%±17.6, p=0,004) with more inflammatory fibrosis at 12 months (1.0%±0.9 vs 0.1%±0.3, p=0,001) (Fig.1). However, the median eGFR was comparable in the 2 groups at 3 months and 12 months, with no significant difference between MMA and control patients in iohexol plasma clearance at 1 year (72.3 vs 75.7 ml/min/1.73m², p=NS). Otherwise, MMA patients had more blood transfusions during the procedure (18/20 vs 5/20, p< 0,00001), more hypovolemia (16/20 vs 9/20, p= 0,02) and more sepsis (8/20 vs 0/20, p=0,001) in the 3 months after KT or LKT, and a higher intrapatient variability (IPV) of plasma calcineurin inhibitor (CNI) levels, during the first month of KT or LKT, with a variation coefficient of 43,6% vs 34,1% (p= 0,029), compared to control patients.
Conclusion: MMA patients KB showed actually an extended and accelerated renal fibrosis in comparison to control patients KB. However, at one year after KT or LKT, the MMA patient GFR is still comparable to control patients. A higher IPV of plasma CNI levels, rate of sepsis and hypovolemia in MMA patients could be a potential explanation of this fibrosis and a new analysis of the data with a control group of LKT patients is ongoing, since 14/20 MMA patients had combined transplantation. Furthermore, direct toxicity of MMA could not be ruled out based on our data and more study on the role of MMA as a promoter of fibrosis are needed.