The implementation process for an electronic pre-visit planning tool: a pediatric kidney transplant quality improvement project
Lindsey Shinn1, Barb Miller4, Kendall Gosch4, Raja Dandamudi2, Vikas Dharnidharka2, Gillian Mayersohn3, Kristin Rich1, Elizabeth Eliopoulos1, Patti Fredrick1.
1Transplant Services, St. Louis Children's Hospital , St. Louis, MO, United States; 2Nephrology, Washington University School of Medicine , St. Louis, MO, United States; 3Psychology, St. Louis Children's Hospital , St. Louis, MO, United States; 4Clinical Systems, Washington University School of Medicine , St. Louis, MO, United States
Introduction: Despite overall improving graft survival rates, recipients still face many post-transplant challenges as a result of immunosuppressive medications and underlying conditions. Specifically, post-transplant medication side effects can lead to changes in body image, weight, and stature, which have been shown to correlate with non-adherence in the pediatric population. These challenges make it important for transplant centers to prolong graft survival time by minimizing immunosuppressive medication side effects and preventing complications caused by non-adherence.
From our own data, 50% of the center’s post 1-year graft failures were due to non-adherence. Given the potential high risk for graft failure due to non-adherence, the transplant team began to identify methods for assessing and intervening with adherence.
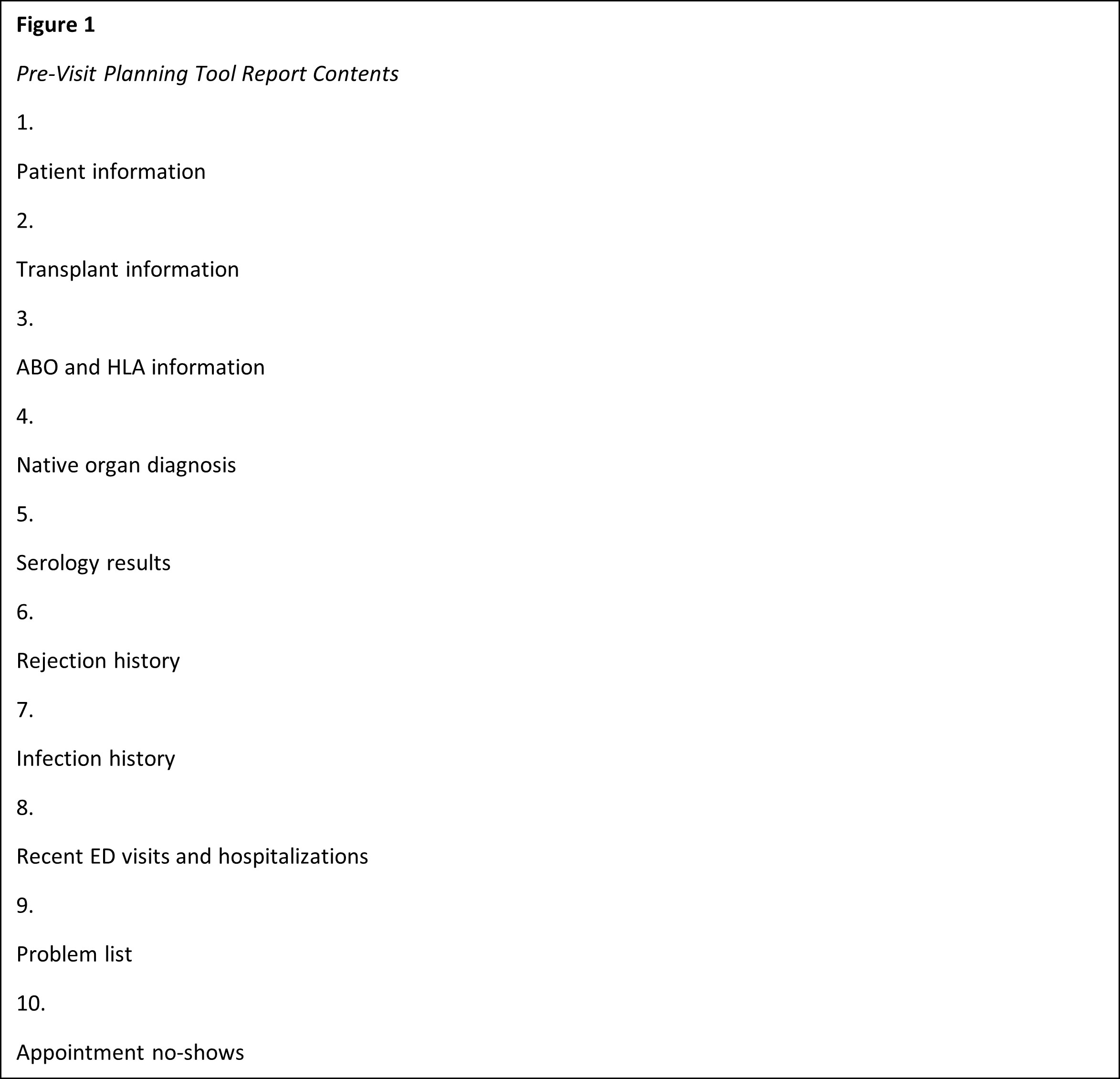
Methods: The team created and implemented an electronic Pre-Visit Planning Tool to assess each patient’s risk of infection/rejection in relation to indicators of suboptimal adherence (see Figure 1). The tool assists the team in building individualized treatment plans and incorporating the appropriate multidisciplinary support during the clinic visit. An implementation plan, consisting of a pre- and post-appointment workflow was created (see Figure 2). The plan involves APNs, MDs, and other multidisciplinary team members (e.g., social work, psychology, pharmacy).
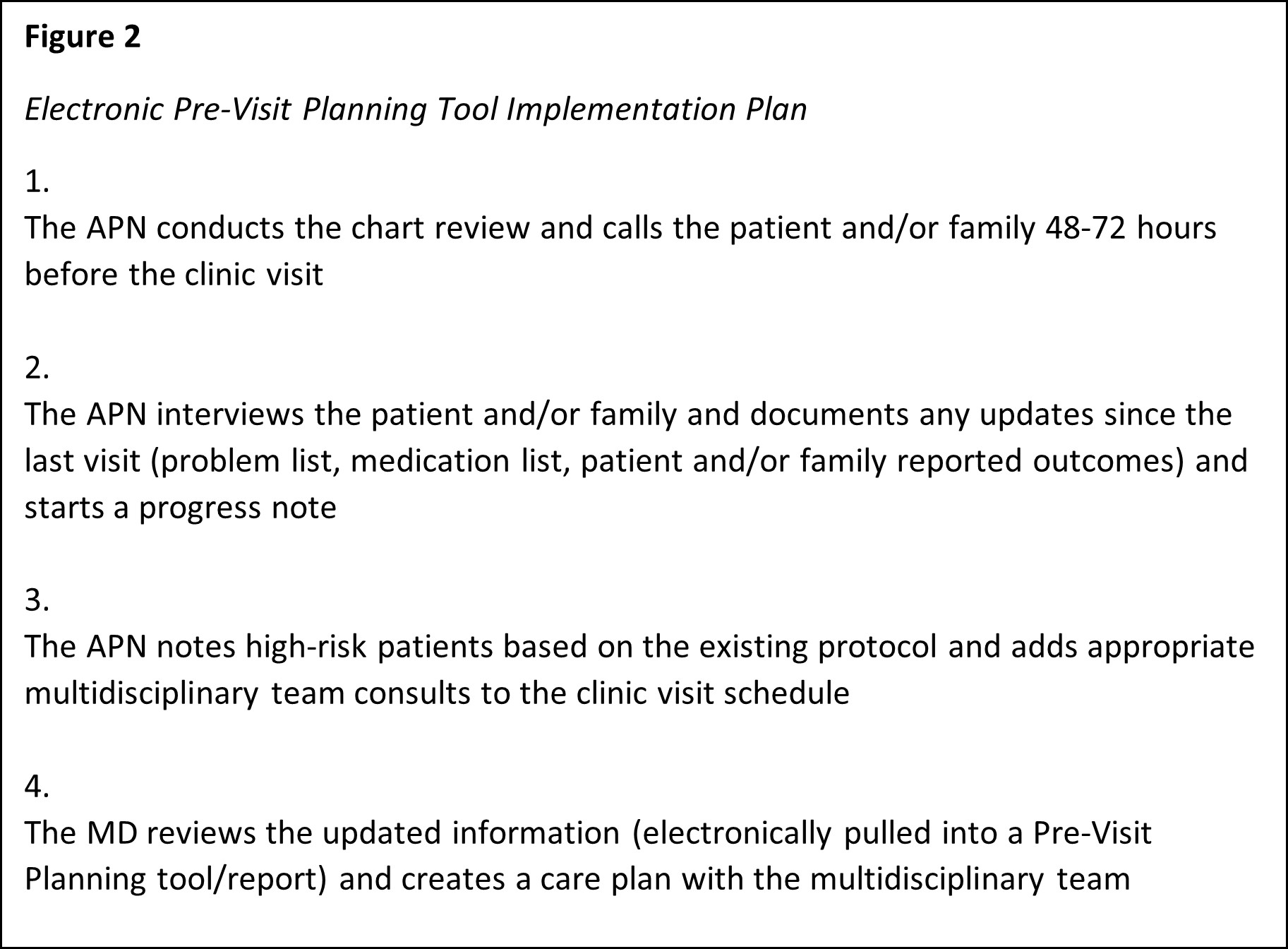
We will track: a) number of times the family was called prior to the clinic visit (within 48-72 hours of visit); b) number of times the tool was used in clinic; c) was a multidisciplinary team member in clinic after being consulted prior?; d) was the follow-up appointment scheduled before leaving?
We will standardize and follow-up on the following: a) gather MD and APN feedback (monthly) b) gather patient/family feedback during patient satisfaction rounding (monthly).
Results: Our goals of this process are to improve, by the July 2023 SRTR release, our 3-year graft survival rates (less than 1.0 hazard ratio and percentage greater than or equal to the U.S. average). We will improve 3-year graft survival rates by achieving: a) rejection rate less than 10%; b) 30-day readmission rate less than 25%.
Conclusion: Successful, long-term outcomes not only rely on effective medication treatment plans, but also take into consideration the child’s physical, emotional, and psychosocial development. In fact, the prevalence of non-adherence in adolescents has been higher than in younger children due to these changes (Kim & Marks, 2014). Focusing on individualized care, such as tailoring immunosuppression medications and assessing the patient’s unique risk for infection/rejection, can help patients prolong graft survival.
Future considerations are to a) track BK, CMV, EBV DNA load results, b) track tacrolimus troughs and medication adjustments, c) incorporate telehealth appointments to minimize family disruption and hospital visits.
[1] Kim, J.J., & Marks, S. Long-term outcomes of children after solid organ transplantation. Clinics. 2014; 69(1): 28-38.