Giant porto-systemic shunt and hepatocellular carcinoma: when liver transplantation is the only solution
Javier Serradilla1, Jose Luis Encinas1, Ane Andrés1, Carlos Andrés De La Torre Ramos1, Karla Estefanía1, María Carolina Sobral1, Esteban Frauca2, Loreto Hierro2, Francisco Hernández Oliveros1.
1Pediatric Surgery, Hospital Universitario La Paz, Madrid, Spain; 2Pediatric Hepatology, Hospital Universitario La Paz, Madrid, Spain
Introduction: Symptoms derived from the presence of a hepatic porto-systemic shunt are variable. Sometimes, it can be silent and not express symptoms clearly for long periods of time. However, its presence can cause a progressive deterioration of the liver which, in advanced cases, could lead to the formation of tumors.
We present the case of a patient who required a liver transplant after presenting with hepatocellular carcinoma in the context of a late-diagnosed giant porto-systemic shunt.
Methods: 16-year-old patient, 75 Kg, who consulted in the Dermatology department for acne treatment. A routine blood test performed before starting treatment found a marked elevation of liver enzymes. Ultrasound showed countless small liver lesions and one large mass (7 x 13 x 9 cm), that resemble regeneration nodules. The CT scan confirmed the findings and revealed a large, almost complete, porto-systemic shunt that left only a filiform portal vein. The biopsy of the large lesion reported the presence of a malignant degeneration compatible with hepatoblastoma. In this context, it was decided to include the patient on the liver transplant waiting list.
Results: The transplant was performed 6 weeks after inclusion.
During transplantation, a nodular liver was observed, with the porto-systemic shunt completely connecting the spleno-mesenteric junction with the infrahepatic vena cava.
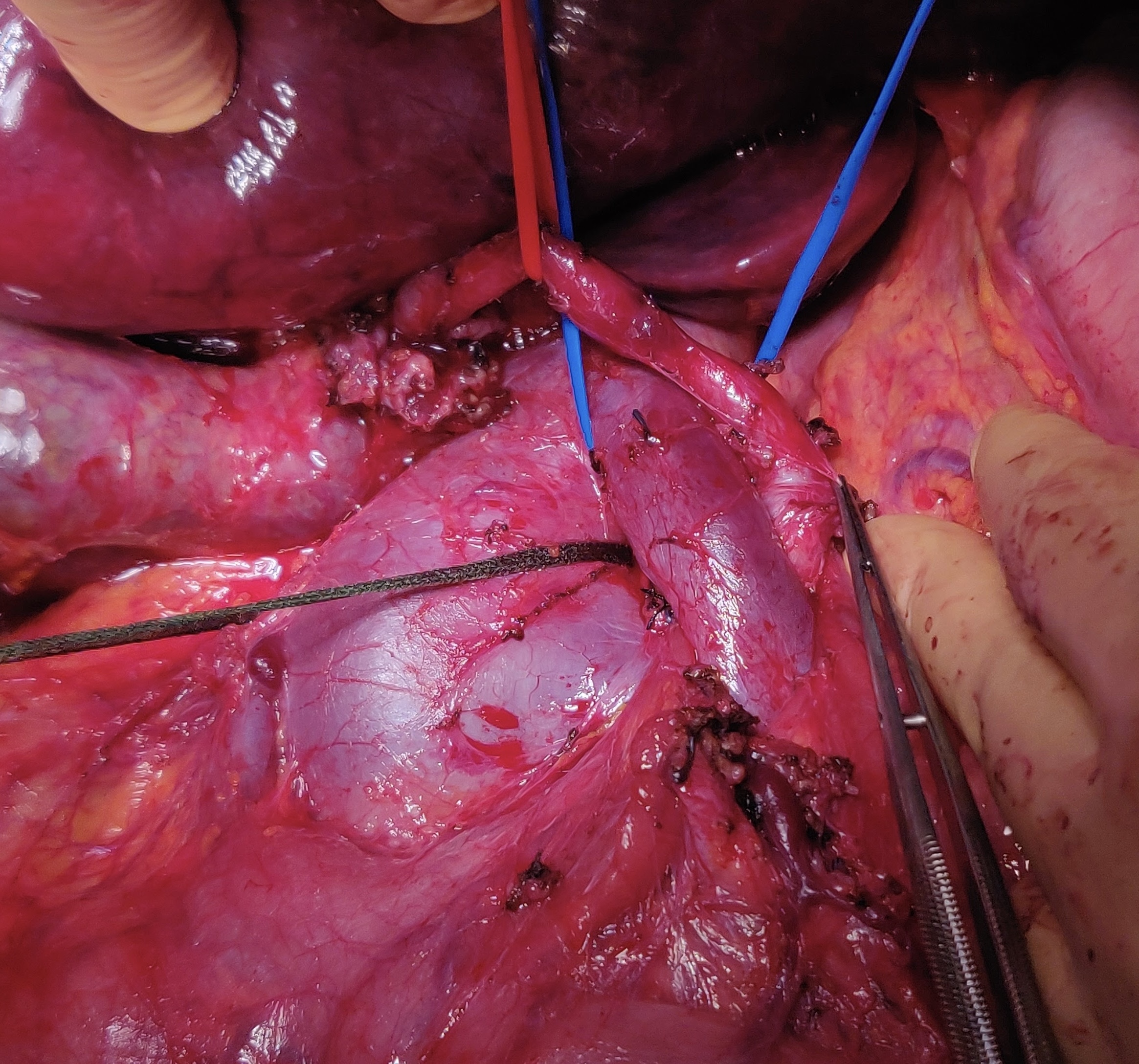
After clamping the inferior vena cava and the shunt completely, it was separated and the lateral wall of the inferior vena cava was closed. The splenomesenteric vessel, previously shunted, was anastomosed end-to-end to the portal vein of the liver graft. Arterial and biliary anastomosis were also performed end-to-end. Pathological examination confirmed the presence of hepatocellular carcinoma.
With 6 months of follow-up, the patient has presented an excellent clinical follow-up, without relevant clinical events.
Conclusion: The presence of a porto-systemic shunt can cause a progressive liver injury that, in advanced cases, could lead to malignancy. Liver transplantation is a feasible therapeutic option in these cases. The shunt must be completely closed to guarantee complete resolution of the symptoms.
Lectures by Javier Serradilla
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Tue-28 09:10 - 10:10 |
Combined Topics | DCD in pediatric transplantation: our multidisciplinary experience | Hill Country CD |
|
Tue-28 09:10 - 10:10 |
Combined Topics | Giant porto-systemic shunt and hepatocellular carcinoma: when liver transplantation is the only solution | Hill Country CD |
