Anjali Khanna-Farber, United States
Clinical Research Coordinator
Pediatric Nephrology
Emory school of Medicine
New onset diabetes after transplant in a single pediatric kidney transplant center
Anjali Khanna-Farber1, Nina J. Ham2, Rochelle Liverman1, Margret Kamel1, Rouba Garro1,3.
1Pediatric Nephrology, Emory school Of Medicine, Atlanta, GA, United States; 2Pediatric Endocrinology, NewYork-Presbyterian / Columbia University Irving Medical Center, New York, NY, United States; 3Pediatric Nephrology, Children's Healthcare of Atlanta, Atlanta, GA, United States
Introduction: The prevalence of new-onset diabetes after transplant (NODAT) in pediatric kidney transplant (KT) recipients varies among studies due to the lack of a consistent definition. Risk factors and pathogenesis associated with its onset are poorly understood.1
The aim of this study is to evaluate the prevalence of and risk factors for NODAT at a high-volume, tertiary care pediatric hospital, and characterize the disease course in NODAT patients.
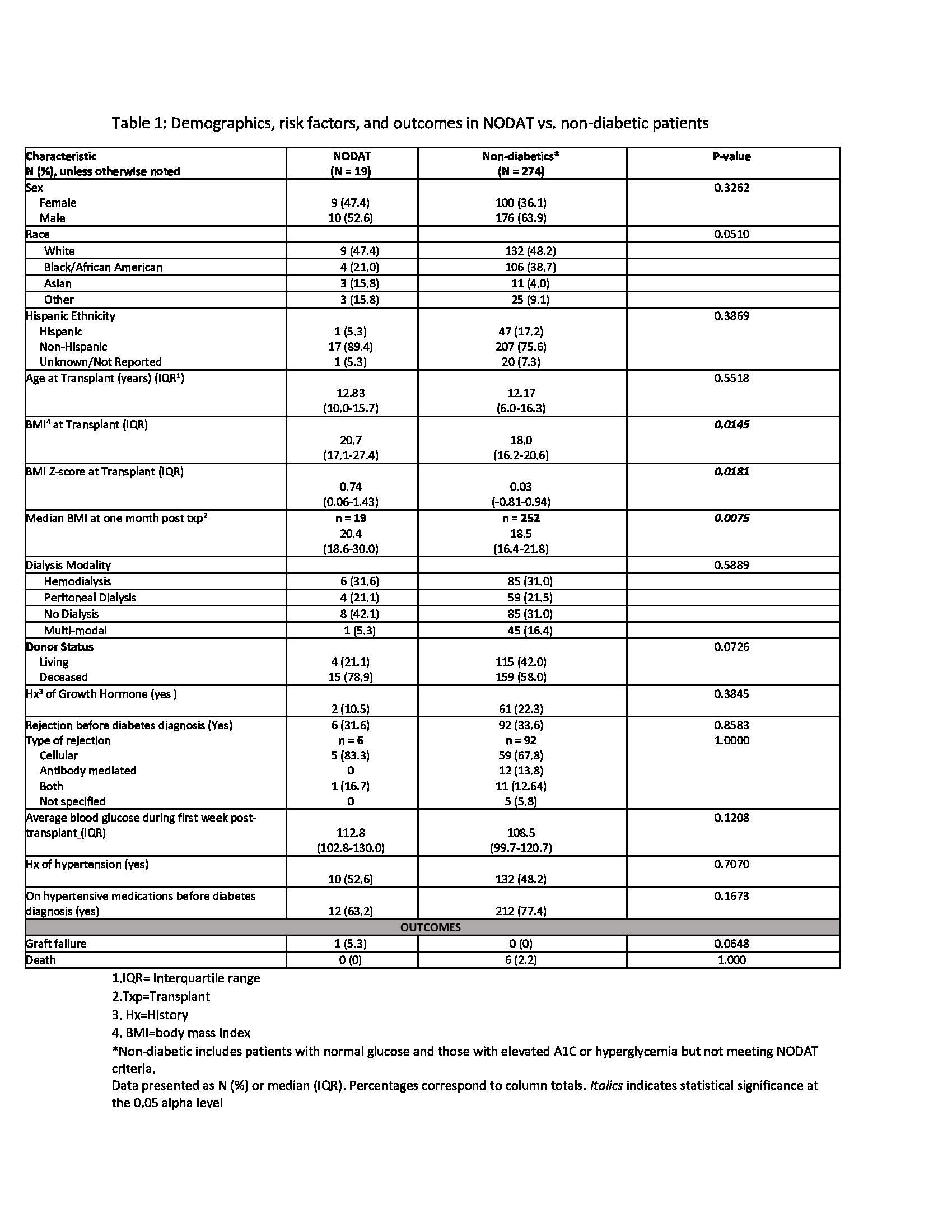
Methods: We performed a retrospective review of pediatric KT recipients transplanted between 2006-2016 at our center. We excluded patients with multi-organ transplants and with pre-existing diabetes. We defined NODAT as persistent hyperglycemia with serum glucose >200 mg/dl, HbA1c >6.5%, and requiring antihyperglycemic medication for ≥ 30 days. We compared demographic and transplant characteristics between NODAT (n=19) and non-diabetic patients (n=274) using Chi-square tests and Wilcoxon rank sum tests. We performed further evaluation of NODAT patients to evaluate risk factors and outcomes.
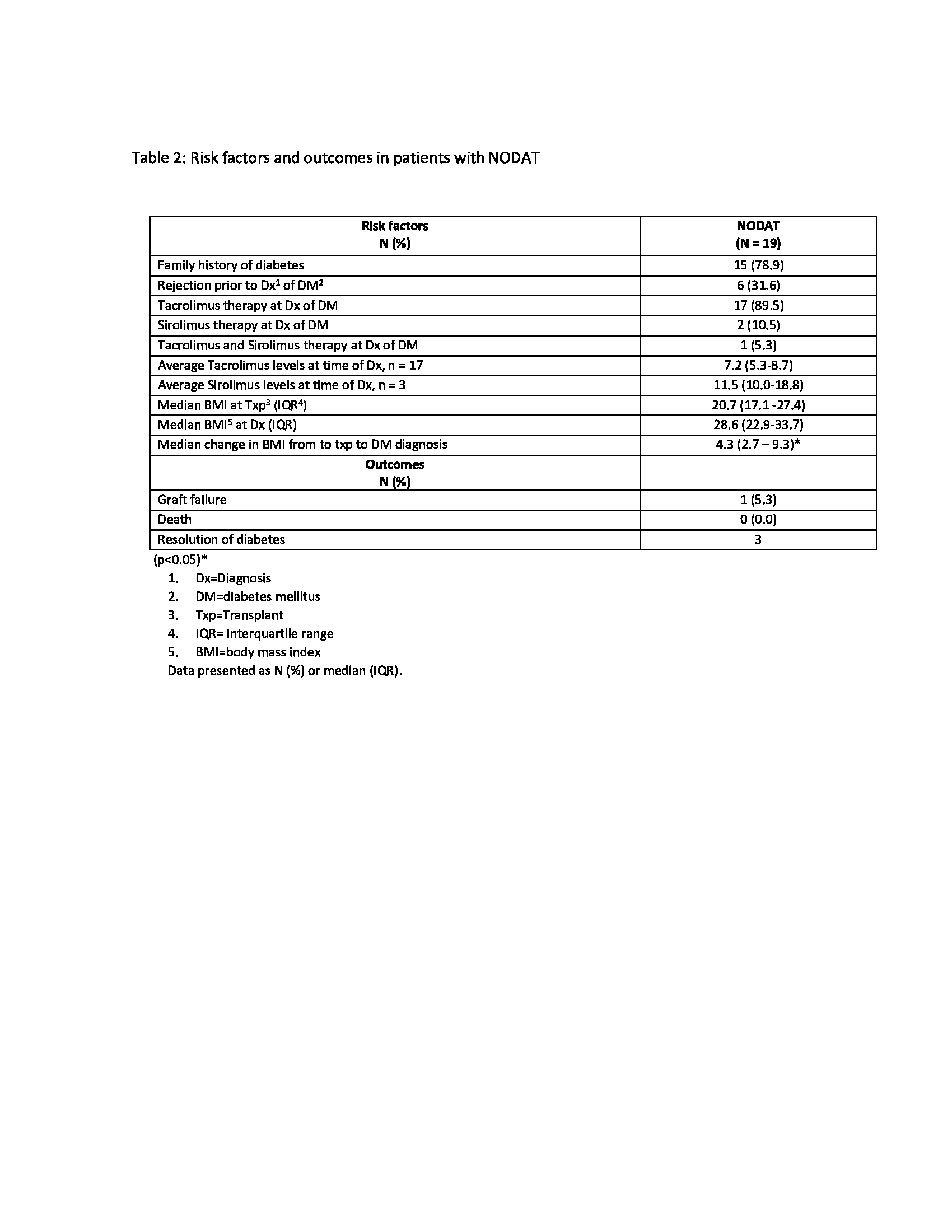
Results: Over the 10-year period, 293 patients met the inclusion criteria with the median age at transplant of 12.8 years. Nineteen patients (6.48%) developed NODAT, 29 patients had elevated HbA1c (5.7-6.4%), 43 patients had hyperglycemia (serum glucose levels 140-199 mg/dl), and 202 patients had normal serum glucose levels. Comparisons of patients with and without diabetes revealed that NODAT patients had higher BMI-Z scores at the time of transplant (p=0.02) (table 1). The median time from transplant to development of NODAT was 17 months (25th-75th: 4 – 83). Most patients who developed NODAT had a family history of diabetes in first-degree relatives (79%), received Deceased Donor KT (78.9%), were maintained on tacrolimus at the time of diagnosis (67%), and had a significant median change in BMI from time of transplant to DM diagnosis (p<0.05) (Table 2). NODAT diagnosis and Insulin initiation occurred in the context of active rejection episodes in three patients. Despite a more stringent definition of NODAT, 2/19 (10%) patients came off insulin therapy and were normoglycemic at 1, 5, and 8 years post DM diagnosis.
Conclusion: A more consistent definition of NODAT and larger studies are warranted to better understand the prevalence, risk factors, and pathogenesis of hyperglycemia and diabetes post-transplant. Further evaluation of the effect of NODAT and glucose intolerance on graft function in this cohort of pediatric KT recipients is underway.
References:
[1] 1. Garro R, Warshaw B, Felner E. New-onset diabetes after kidney transplant in children. Pediatric Nephrology. 2014;30(3):405-416. doi:10.1007/s00467-014-2830-7
Lectures by Anjali Khanna-Farber
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Sat-25 18:00 - 19:15 |
P6- Kidney Posters | New onset diabetes after transplant in a single pediatric kidney transplant center | Zilker 1-2 |
