Jorge A. Sanchez Vivaldi, United States
Kidney and Liver Transplant Surgery Fellow
Division of Surgical Transplantation
University of Texas Southwestern Medical Center
Imperfect pre-recovery liver biopsies in pediatric liver transplantation: How do they fare?
Jorge Sanchez Vivaldi1,2, Madhukar S. Patel1,2, Benjamin K. Wang1, Andrew Shubin1, Yash Kadakia1, Dev M. Desai1,2, Jigesh A. Shah1,2, Malcolm MacConmara1,2, Steven Hanish1, Parsia Vagefi1, Christine S Hwang1,2.
1Department of Surgery, Division of Surgical Transplantation, University of Texas Southwestern Medical Center, Dallas, TX, United States; 2Department of Surgery, Division of Surgical Transplantation, Children's Medical Center, Dallas, TX, United States
Introduction: Immaculate liver allografts are commonly utilized in pediatric transplantation. On the other hand, outcomes of pediatric livers with imperfect pre-recovery biopsies are not well described. We queried if the outcomes of imperfect livers transplanted in pediatric recipients is comparable to livers with normal biopsies and if utilization of the imperfect allografts is warranted to help expand the donor pool.
Methods: We examined the STARfile and evaluated all deceased donor liver allografts with biopsies that were transplanted into pediatric recipients between January 2015 and December 2020. Pediatric recipients were defined as those transplanted before 18 years of age. Imperfect liver biopsy (IL) allografts were defined as those with >5% macrosteatosis, any fibrosis and/or any inflammation. Normal liver biopsy (NL) allografts were defined as those with <5% macrosteatosis, no fibrosis and no inflammation. Donor and recipient demographic data were examined, as were survival and outcomes. A p-value of <0.05 was significant.
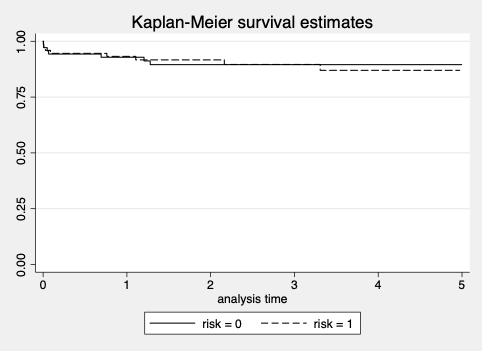
Results: There were 155 biopsied liver allografts in the study period. Of those, 74 met IL criteria and 70 were NL criteria. Donors of IL grafts were older when compared to NL livers (22.7 +/- 18.6 y vs. 14.4 +/- 15.7 y, p<0.004). Donor BMI (1.5 +/- 0.4 vs. 1.5 +/- 0.3, p<0.57) and DRI (20.6 +/- 5.5 vs. 22.0 +/- 6.1, p<0.15) were similar in both groups, NL vs. IL, respectively. When examining biopsy data, the average macrosteatosis percentage was 0.8 +/- 1.8 vs. 8.4 +/- 12.3, NL vs. IL, respectively (p<0.001). The IL group had 11/74 (14.9%) with any fibrosis and 48/74 (64.9%) with any inflammation. Recipient age was greater in the IL group compared to the NL group (7.7 +/- 6.4 y vs. 5.6 +/- 5.9 y, p<0.039). PELD scores were also higher in the IL group (18.2 +/- 15.3 vs. 12.9 +/- 14.1, p<0.032). There were no significant differences in length of stay post-transplant and allograft outcomes were similar between the two groups (Table 1). Long term liver allograft survival were comparable between the two groups (Figure 1).
Conclusion: Pediatric patients transplanted with IL deceased donor liver allografts had similar outcomes compared to those who received NL livers. The use of IL liver grafts can be a viable option for pediatric recipients, potentially ameliorating the organ shortage.

References:
[1] Rie Irie, Atzuko Nakazawa, et al. Outcome for Pediatric Recipients of Macrosteatotic Liver Grafts From Living Donors. Liver Transplantation. 2020 Jul;26(7):899-905.
[2] Peter J. Altshuler, et al. Evaluating Outcomes Related to Donor and Recipient Metabolic Environment: Macrosteatotic Allografts and Nonalcoholic Steatohepatitis. Liver transplantation. 2022 Apr;28(4):623-635.
[3] Malik T, Joshi M, Godfrey E, et al. Pediatric discard risk index for predicting pediatric liver allograft discard. Pediatr Transplant. 2021;25:e13963
[4] Purvis JW, Orandi BJ, Dhall D, et al. Hepatic macrosteatosis in the US pediatric deceased liver donor population. Pediatr Transplant. 2022;26:e14155.
Lectures by Jorge A. Sanchez Vivaldi
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Sat-25 18:00 - 19:15 |
P4- Immunosuppression Posters | Belatacept-based immunosuppression in pediatric kidney transplantation | Zilker 1-2 |
|
Tue-28 09:10 - 10:10 |
Liver | Imperfect pre-recovery liver biopsies in pediatric liver transplantation: How do they fare? | Hill Country AB |
