Paediatric Gastroenterology/Hepatology
University of Witwatersrand, Faculty of Health sciences
Charlotte Maxeke Johannesburg Academic Hospital
Disparity in organ distribution in South Africa
Anja Meyer1,3, Sechaba T. Palweni1,2,3, Nolitha Pikela1,3, Thembeka Jama1,3, Nancy Makoe1,3, Priya Walabh3,4,5.
1Surgery, Charlotte maxeke Johannesburg Academic Hospital, Johannesburg, South Africa; 2Surgery, University of Witwatersrand, Faculty of Health Sciences, Johannesburg, South Africa; 3Gauteng Solid Organ Transplant Governance, Gauteng Department of Health, Johannesburg, South Africa; 4Paediatrics and Child Health, University of Witwatersrand, Faculty of Health Sciences, Johannesburg, South Africa; 5Paediatric Gastroenterology, Hepatology and Nutrition, Charlotte maxeke Johannesburg Academic Hospital, Johannesburg, South Africa
Introduction: In South Africa (SA), there is a significant healthcare disparity with 84% of the population accessing state sector government facilities and 16% of the population accessing private healthcare facilities through personal medical insurance. S.A has a comparatively low deceased donation rate at 3 per million population. The lack of clear governmental policies on allocation has resulted in lack of standardization and discrepancy in distribution of solid organs. The objective of our study was to determine the contribution of state sector to deceased organ donation in Gauteng province in SA and assess the distribution of various organs between public and private health sectors. We also evaluated the effect of the Covid 19 pandemic on organ donation and allocation.
Methods: We undertook a retrospective registry review of consented brain-dead donors from state sector within the Gauteng Province from the 1 January 2016 till 30 June 2021. Permission was obtained from the University of Witwatersrand HREC (M211045)
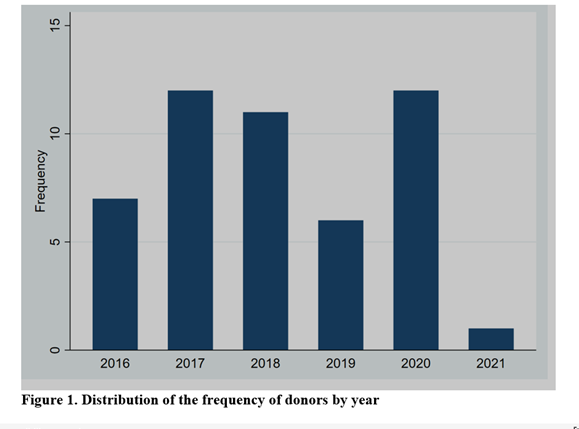
Results: The records of 49 deceased donors were reviewed and analyzed. The mean donor age at the time of death was 31.5 years with the age group 30-39 years constituting majority of deceased donors at 15/49 (30.6%). Most donors were male (75.5%) with black and white races contributing the most donations at 43% and 41% respectively. Fifteen (15/49: 30.6%) donor hearts were suitable for cardiac transplantation with 12/15 (80%) allocated to private sector recipients in Gauteng and the rest to state sector (Cape Town). Lungs were distributed between private sector in Gauteng (6/11: 55%) and state sector in Cape Town (5/11: 45%). Thirty-five livers (71.4%) were found suitable and used for recipients in the private sector with 5/49 (10.2%) used for state sector patients. Four (6.2%) of livers were split and donated between private and public sector patients. Two kidneys were donated from each of the 49 donors which were distributed relatively equally between the 2 sectors. (Table1a) The median age of liver transplant recipients was higher in the private sector at 45years (IQR 39-59) compared to the public sector at 21 years (IQR17-34) and this difference was statistically significant (P =0.044). There was a significant difference in proportion of kidneys allocated to pediatric recipients before and after 1 March 2020 (P < 0.001)
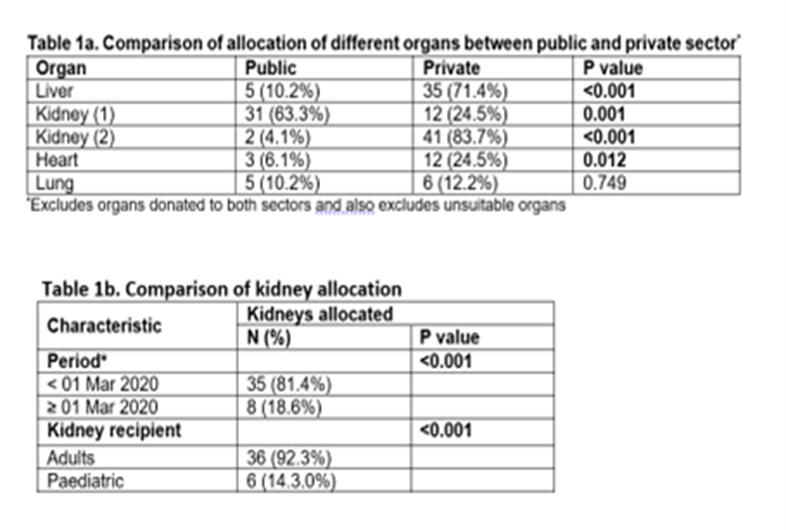
when there was a transition from a private sector-based waitlist to an independent state sector wait-list with a kidney transplantation unit being established in state sector. Lower proportions of deceased donations were observed during the Covid 19 pandemic, and these differences were statistically significant for all solid organs.
Conclusion: Definite disparity exists in the distribution of solid organs in SA, between health sectors and between the pediatric and adult population. Redistribution of healthcare resources and clarity of regulations governing organ transplantation in SA is required.
References:
[1] Moosa MR. The state of kidney transplantation in South Africa. South African Med J. 2019;109(4):235-240. doi:10.7196/SAMJ.2019.v109i4.13548
[2] Davidson B, Toit T Du, Jones ESW, et al. Outcomes and challenges of a kidney transplant programme at Groote Schuur Hospital, Cape Town: A South African perspective. PLoS One. 2019;14(1):1-15. doi:10.1371/journal.pone.0211189
[3] Labuschagne D, Carstens P. An analysis of organ transplantation in South Africa with specific reference to organ procurement. Thesis Submitt Partial fulfilment Requir degree master laws Fac law Univ Pretoria. 2013;(October).
[4] Lauerer M, Kaiser K, Nagel E. Organ Transplantation in the Face of Donor Shortage - Ethical Implications with a Focus on Liver Allocation. Visc Med. 2016;32(4):278-285. doi:10.1159/000446382
Lectures by Priya Walabh
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Sun-26 10:00 - 11:00 |
Ethical/Psychosocial and Economical Issues | Disparity in organ distribution in South Africa | Hill Country CD |
|
Sat-25 18:00 - 19:15 |
P5- Infectious Diseases Posters | Epstein Barr Virus risk stratification as a tool to predict post-transplant lymphoproliferative disorder in pediatric liver transplant recipients | Zilker 1-2 |
