First case report of multivisceral transplant from a deceased cardiac death donor
Ane Andres1,7, Jose Luis Encinas1, Alba Sanchez-Galan1, Javier Serradilla1,7, Karla Estefania1, Rocio Gonzalez-Sacristan2, Alida Alcolea2, Pilar Serrano2, Belen Estebanez5, Iñigo Velasco4, Paula Burgos4, Alvaro Gonzalez-Rocafort4, Bunty Ramchandani4, Belen Calderon-Llopis3, Cristina Verdu3, Paloma Talayero6, Pablo Stringa 7, Esther Ramos2, Francisco Hernandez-Oliveros1,7.
1Pediatric Surgery, Hospital La Paz, Madrid, Spain; 2Pediatric Gastroenterology. Intestinal Rehabilitation Unit, Hospital La Paz, Madrid, Spain; 3Pediatric Intensive Care Unit, Hospital La Paz, Madrid, Spain; 4Pediatric Cardiac Surgery Department, Hospital La Paz, Madrid, Spain; 5Transplant Coordination Unit, Hospital La Paz, Madrid, Spain; 6Immunology Department, Hospital 12 de Octubre, Madrid, Spain; 7Research Institute, Hospital La Paz, Madrid, Spain
A shortage of pediatric multivisceral donors accounts for the long time and mortality on the waiting list (WL) of pediatric patients. The use of donors after cardiac death (DCD), especially after the outbreak of normothermic regional perfusion (NRP), has increased in recent years for all solid organs, except for the intestine, mainly because of the higher susceptibility to ischemia-reperfusion injury.
We present the first case in the literature of multivisceral DCD transplantation in a 13-month-old recipient (4 kilograms) with ultra-short bowel syndrome from a 2.5-month-old donor with irreversible epileptic status.
After the decision to limit therapeutic efforts and obtaining ethical and legal authorization, the patient was taken to the operation room accompanied by their parents.
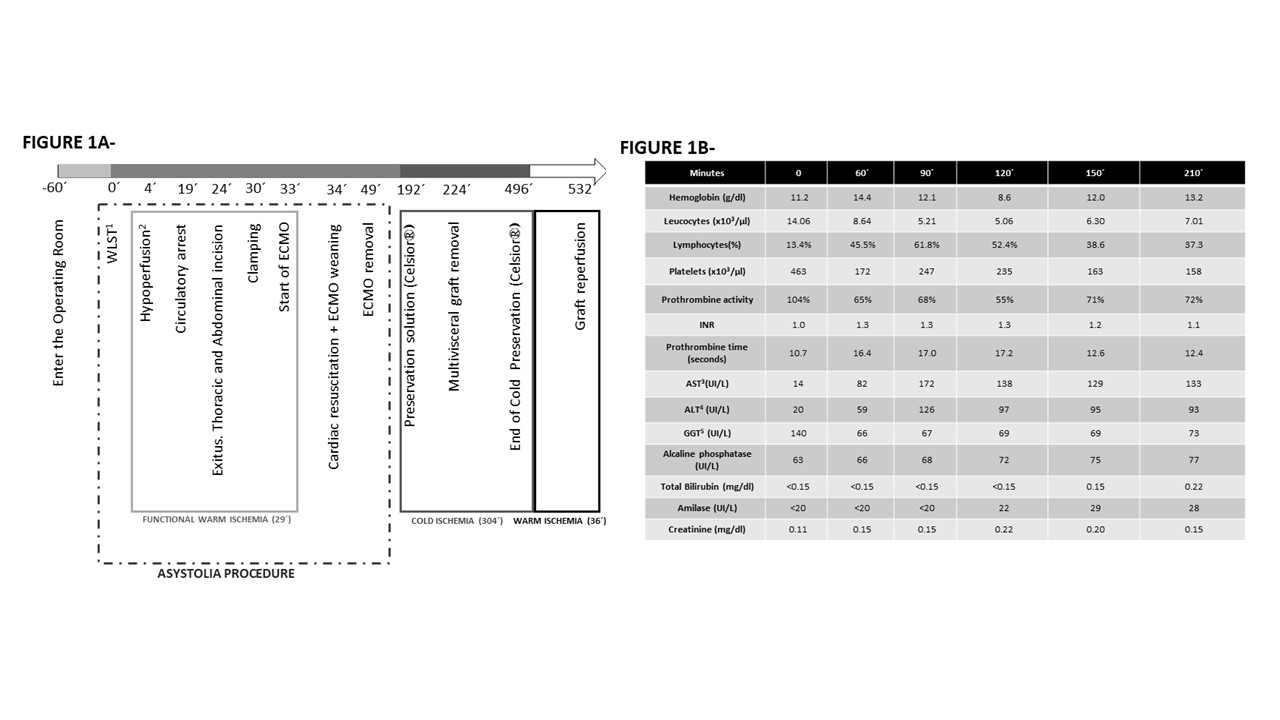
Once exitus was certified an extracorporeal membrane oxygenation (ECMO) circuit was established cannulating the aorta and infrarenal vena cava, whereas the supra-aortic branches were clamped. The heart was recovered by the cardiac team and the abdominal organs completely recovered from ischemia through NRP (ECMO initially and beating heart later) (Figure 1A and 1B).
After perfusion with the preservation solution, the multivisceral graft was uneventfully implanted (Figure2).
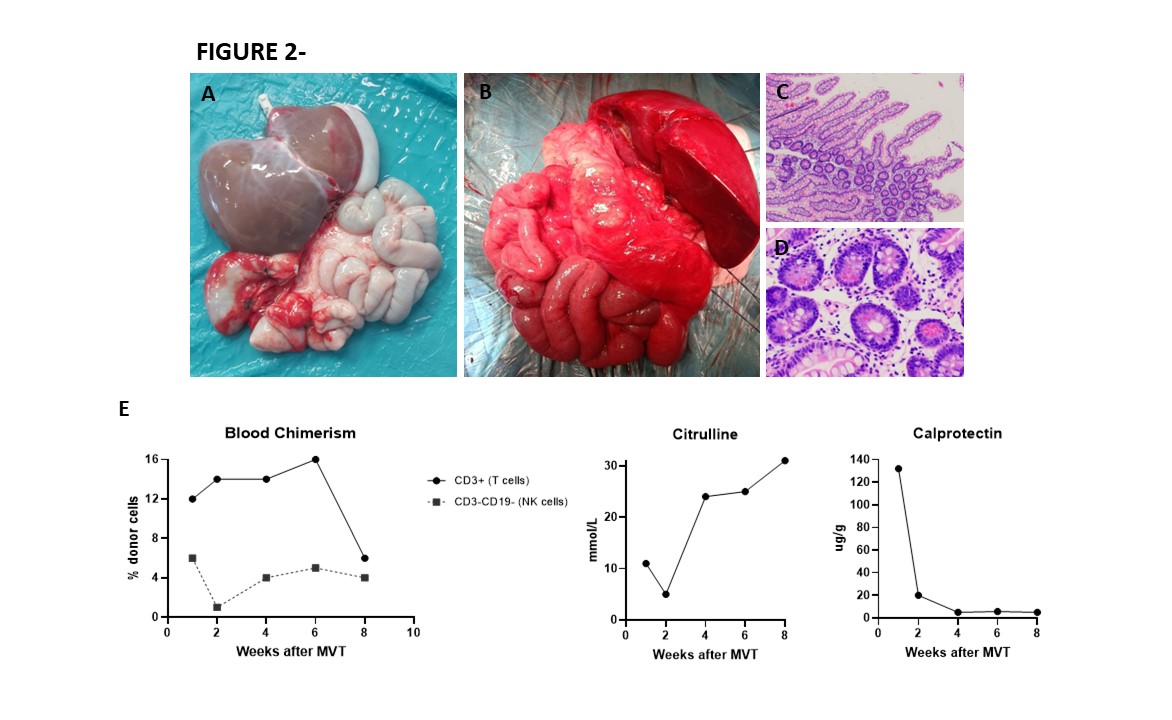
Two months later, the patient was discharged without any complications.Three months after transplantation, the patient was home, eating by mouth, asymptomatic (5.1 kg), with stable tacrolimus levels and digestive losses of approximately 55 mL/kg/day, although still on PN for a catch-up, with a view to its withdrawal in the coming weeks.
This case opens the possibility of reducing the time spent on WL and mortality for these patients.
Mutua Madrileña Foundation, Idipaz, ONT; NUPA.
[1] Guo M, Lu C, Li L, Yao D, Li Y. Normothermic extracorporeal membrane oxygenation support: Improving the function of intestinal grafts obtained from cardiac death donors. Artif Organs. Oct 2020;44(10):1098-1106. doi:10.1111/aor.13697
[2] Miñambres E, Suberviola B, Dominguez-Gil B, et al. Improving the Outcomes of Organs Obtained From Controlled Donation After Circulatory Death Donors Using Abdominal Normothermic Regional Perfusion. Am J Transplant. Aug 2017;17(8):2165-2172. doi:10.1111/ajt.14214
[3] Venick RS, Duggan E, Whatley J. Current status of pediatric intestinal transplantation in the United States. Curr Opin Organ Transplant. 04 2020;25(2):201-207. doi:10.1097/MOT.0000000000000744