Optimizing Vaccinations in Pediatric Kidney Transplant Patients
Jessica Brennan1, Marilyn McEnhill1.
1Department of Surgery, Division of Transplant , UCSF Benioff Children's Hospital, San Francisco, CA, United States
Introduction: Vaccine-preventable infections occur among solid organ transplant recipients. The aims of this quality improvement project were to review our center’s pediatric kidney transplant vaccination data and develop strategies to improve vaccination rates consistent with the 2019 guidelines from the American Society of Transplant (AST) Infectious Diseases Community of Practice.
Methods: We performed a retrospective chart review of pediatric kidney transplant recipients who received an allograft from 2015 to 2020. A total of 57 patients were studied, we excluded deceased patients and patients who transitioned their care to the adult transplant service. Vaccination records were audited. The subject age range was 2-23 years. The 2019 AST vaccination guidelines were used as a model for vaccine recommendations, in addition to the Center for Disease Control (CDC) vaccine schedules.
Pediatric Vaccine Audit
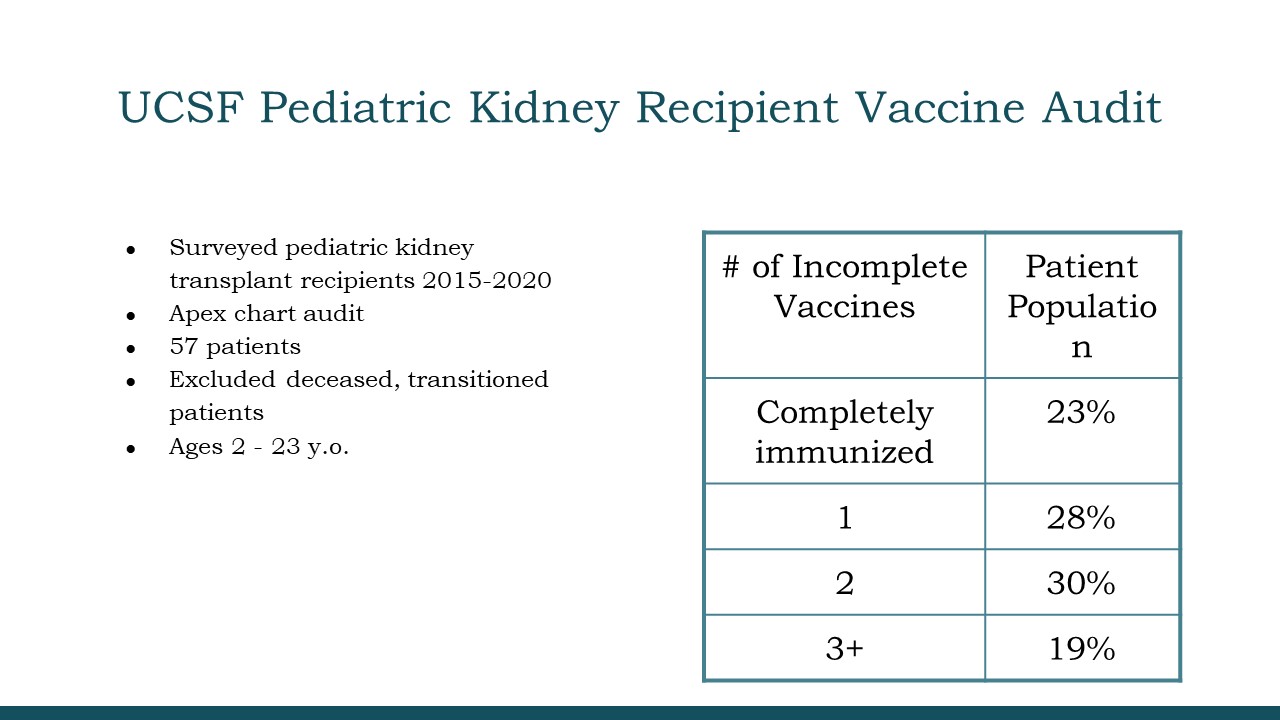
Results: A total of 23% of our study population was completely immunized. Of the remaining patients, just under 20% were missing three or more vaccines. There was 100% influenza vaccine compliance with patients seen for in person clinic visits. Of the five patients that did not receive the influenza vaccine, two refused to receive the influenza vaccination.
Of the 45 patients with incomplete vaccinations, we found that the most frequently missed vaccines were the third dose of the human papillomavirus (HPV) and the second dose of the meningococcal (MCV ACYW) vaccine. A total of twenty patients were missing one of the pneumococcal vaccines (PCV-13 or PPSV 23 valent).
In the < 6-year-old group, patients were found to be missing both transplant specific vaccinations and CDC age-based vaccinations. In the adolescent group (age 12-16 years old), almost 40% did not complete the 3 dose HPV series. Most completed at least 1 or 2 vaccines prior to transplantation. Approximately 30% of this group, were missing one or both meningococcal vaccines.
Meningococcal and pneumococcal and vaccines accounted for almost 40% of missing vaccines among patients aged 17-23. Most were vaccinated with the 7-valent pneumococcal vaccine in early childhood, but a portion did not receive the additional pneumococcal vaccines.
Conclusions: Vaccination of pediatric kidney transplant recipients is critical in preventing illness related complications. Our findings highlight the problem of incomplete vaccinations in this population for both CDC age-based and transplant specific vaccinations. These findings led our group to implement strategies to improve vaccination rates for the kidney transplant population with an emphasis on completing vaccinations prior to transplant and forming a working group with our pediatric ID colleagues. Next we focused on our partnerships with PCPs and to develop electronic medical record tools to identify gaps implementing vaccinations. Reassessment of vaccination rates will be performed 12-18 months following the implementation of these strategies.
[1] References: [1] Danziger-Isakov L, Kumar D. Clinical Transplantation. 2019; 33(9):e13563. Vaccination of solid organ transplant candidates and recipients: Guidelines from the American society of transplantation infectious diseases community of practice.
[2] Feldman A., Beaty B. Curtis, D. JAMA Pediatrics. 2019;173(3):260-268. Incidence of Hospitalization for Vaccine-Preventable Infections in Children Following Solid Organ Transplant and Associated Morbidity, Mortality, and Costs