Using Renal Genetics in the Pediatric Kidney Transplant Evaluation
Jessica Brennan1, Megan Schoettler2, Sanober Sadiq2, Farzana Perwad2.
1Department of Surgery, Division of Transplant , UCSF, Benioff Children's Hospital , San Francisco, CA, United States; 2Department of Pediatrics , UCSF Benioff Children's Hospital , San Francisco, CA, United States
Introduction: Renal biopsy is the mainstay of renal pathological diagnosis. Biopsies can be costly and painful and may not always yield a precise diagnosis. Our aim was to develop a Pediatric Renal Precision Medicine program to better identify genetic causes of kidney disease for patients undergoing a pre-transplant evaluation.
Background: In 2018 at University of California, San Francisco we developed a Renal Precision Medicine Program to better understand, manage and treat children with genetic causes of chronic kidney disease (CKD). Advancements in gene sequencing technology has enabled rapid discovery of genetic causes of CKD. Prior to the inception of this program, ordering genetic testing on patients with chronic kidney disease was a lengthy and complex process. The collaboration between pediatric nephrology and genetics teams will be described to improve the workflow.
Program goals: Decrease length of time to obtain genetic testing.
Improve understanding of genetic causes of CKD.
Develop a workflow for patients to be tested and seen by both nephrology and genetics simultaneously when appropriate.
Utility of genetic testing in pre transplant evaluation
Known alterations on treatment strategy based on genetic testing
Recurrence
•20%–30% FSGS disease-recurrence after kidney transplantation;
•Risk is only 4%–8% in patients who have genetic forms of SRNS.
Immunosuppression
Regimens can be adjusted for patients who have genetic causes of SRNS.
Candidates for a steroid minimization protocol at the time of transplantation given their low risk for immunologic disease
Need for Nephrectomy
Can avoid nephrectomy in genetic SRNS if being done to monitor recurrence post transplant
Living Donation
Genetic FSGS- living donation is acceptable
Alport syndrome– screen donors to exclude those with positive mutations
Other features
Screen for extrarenal manifestations/organ involvement to provide anticipatory guidance for clinical management
Identify need for combined liver kidney transplant (Primary hyperoxaluria, aHUS)
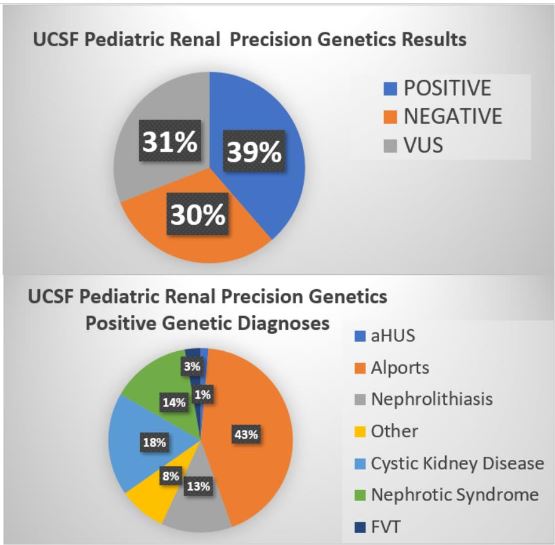
UCSF Pediatric Renal Precision Genetics Program Development and Workflow
Medical genetics physician was identified and became a program champion. All new CKD patients were given access to timely genetic testing. Monthly clinic established and staffed by nephrology and genetics. Patients reviewed prior to scheduling by nephrology nurse practitioner
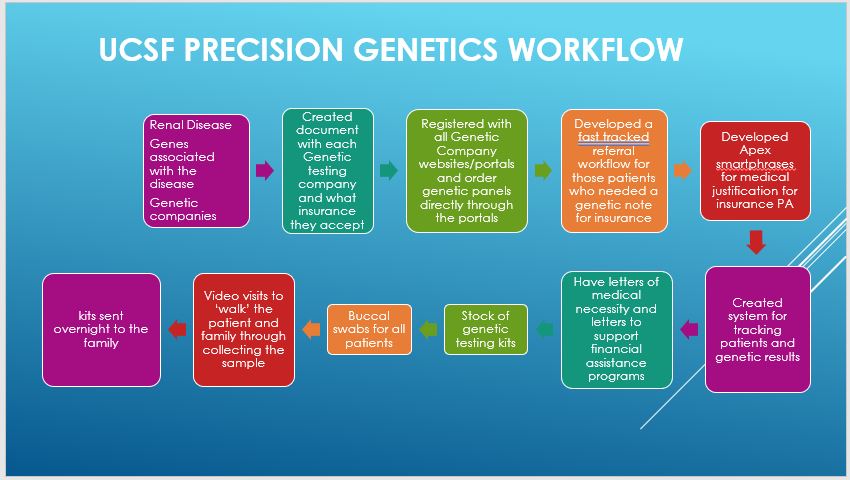
Conclusion: Shorter referral time was achieved through a combined clinic. This decreased the length of time from referral to being seen from 6 months to one month. Genetic testing and results communicated rapidly to the patient. Use of early genetics testing may guide the course to successful transplant among pediatric kidney transplant candidates.
Balram Gangaram, MBBS Assistant Clinical Professor University of California San Francisco Division of Medical Genetics- Department of Pediatrics.
[1] Murray SL, Dorman A, Benson KA, Connaughton DM, Stapleton CP, Fennelly NK, Kennedy C, McDonnell CA, Kidd K, Cormican SM, Ryan LA, Lavin P, Little MA, Bleyer AJ, Doyle B, Cavalleri GL, Hildebrandt F, Conlon PJ. Utility of Genomic Testing after Renal Biopsy. Am J Nephrol. 2020;51(1):43-53. doi: 10.1159/000504869. Epub 2019 Dec 10. PMID: 31822006; PMCID: PMC6957728.
[2] Groopman EE, Marasa M, Cameron-Christie S, Petrovski S, Aggarwal VS, Milo-Rasouly H... Gharavi AG. Diagnostic Utility of Exome Sequencing for Kidney Disease. N Engl J Med. 2019 Jan 10;380(2):142-151. doi: 10.1056/NEJMoa1806891. Epub 2018 Dec 26. PMID: 30586318; PMCID: PMC6510541.